As clinicians on the front lines of the opioid and stimulant crisis, we know that methamphetamine use disorder presents unique challenges not just in treatment, but in how we document and code these conditions.
Whether you're a psychiatrist managing complex addiction cases, a primary care physician encountering stimulant use in your practice, or an emergency medicine physician treating acute intoxication, understanding the nuances of methamphetamine-related ICD-10 codes is essential for accurate clinical documentation.
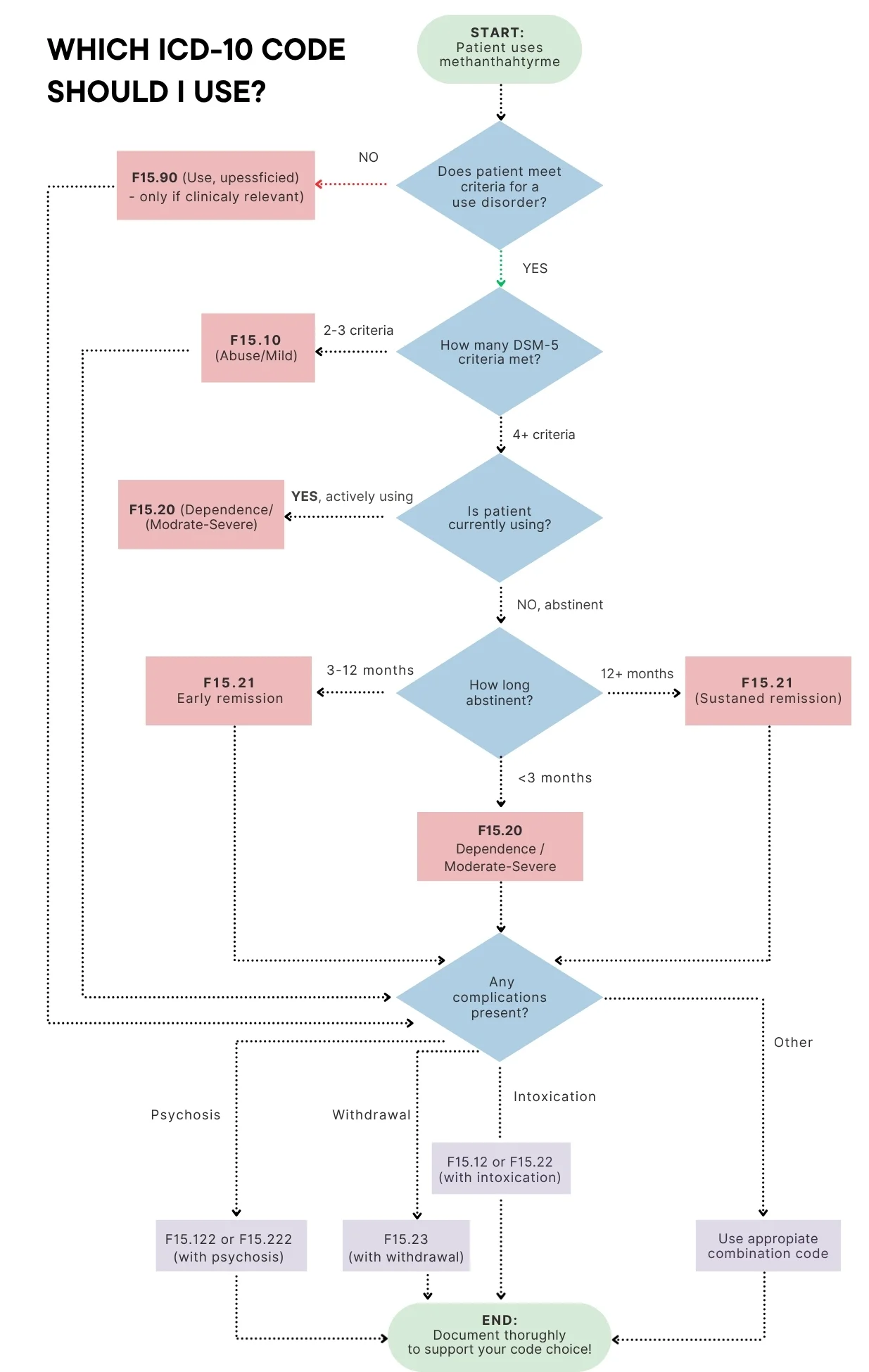
Let be direct: the ICD-10 code for methamphetamine use isn't a single code. It's a family of codes that reflect the spectrum of severity, complications, and clinical presentations we encounter. Getting this right matters for patient care, treatment planning, and ensuring your documentation supports the medical necessity of interventions.
Clear documentation helps translate clinical reality into the correct ICD-10 code, ultimately supporting patient care and meeting regulatory requirements.
Understanding the Core ICD-10 Codes for Methamphetamine Use Disorder
The methamphetamine use disorder ICD-10 codes fall under the F15.xxx category—"Other stimulant related disorders." Here's what you need to know about the primary codes:
F15.10 – Other Stimulant Abuse, Uncomplicated
This code represents what we now call mild methamphetamine use disorder. Use F15.10 when your patient's methamphetamine use is causing negative consequences but hasn't reached the threshold of dependence. Clinically, this means the patient meets 2-3 DSM-5 criteria, perhaps they're using more than intended and it's affecting work performance, but they haven't developed significant tolerance or withdrawal symptoms.
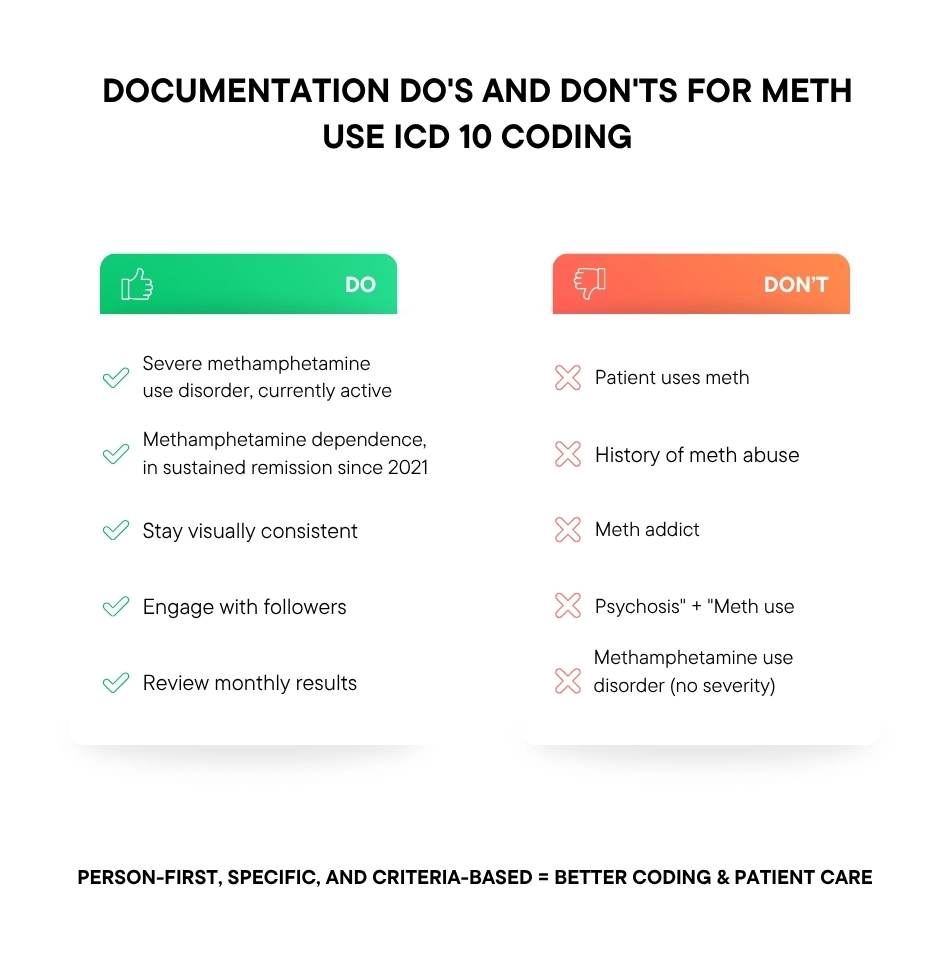
Documentation tip: Be specific about which criteria the patient meets. For example: "Mild methamphetamine use disorder (meets 3 criteria: recurrent use despite work conflicts, unsuccessful quit attempts, continued use despite relationship problems)."
F15.20 – Other Stimulant Dependence, Uncomplicated
The F15.20 code is your go-to for moderate to severe methamphetamine use disorder. This represents patients with significant impairment those who have developed tolerance, experience withdrawal, have made multiple unsuccessful attempts to quit, and whose lives are substantially impacted by their methamphetamine use.
When you're documenting for F15.20, you're describing a patient who meets 4 or more DSM-5 criteria (4-5 for moderate, 6+ for severe). These are the patients who need intensive intervention, whether that's residential treatment, intensive outpatient programs, or comprehensive psychiatric care.
F15.21 – Other Stimulant Dependence, In Remission
Here's where documentation becomes crucial for the history of methamphetamine abuse ICD-10 coding. When a patient has achieved sustained abstinence, typically 12 months or more, F15.21 is the appropriate code. This isn't just a historical note; it's an active diagnosis that recognizes the patient's recovery status while acknowledging the chronic nature of addiction.
Critical distinction: Don't just write "history of methamphetamine abuse" in your problem list. Instead, document: "Methamphetamine dependence, in sustained remission since [date]." This specific language ensures proper coding and communicates the patient's current status to other providers.
For patients with a history of mild use disorder now in remission, the analogous code is F15.11 (abuse in remission).
F15.90 – Other Stimulant Use, Unspecified
The ICD-10 code for methamphetamine use, unspecified (F15.90-F15.99 range) should be your last resort. Use these codes only when you've documented methamphetamine use that's relevant to the clinical encounter but you cannot determine whether it constitutes abuse or dependence.
For example: A patient admitted for chest pain reports occasional methamphetamine use, but you don't have sufficient information to diagnose a use disorder. You might use F15.90 to capture that the substance use is clinically relevant to the presentation.
Warning: Overusing unspecified codes suggests incomplete documentation. If you're evaluating a patient, take the time to assess whether they meet criteria for a use disorder. Your documentation should rarely default to "unspecified."
The ICD-10 Coding Hierarchy: Why Specificity Matters
Here's a critical rule that affects how your documentation translates to codes: ICD-10 follows a severity hierarchy. If you document both "abuse" and "dependence" for the same substance, only dependence gets coded. The hierarchy is:
Dependence > Abuse > Use
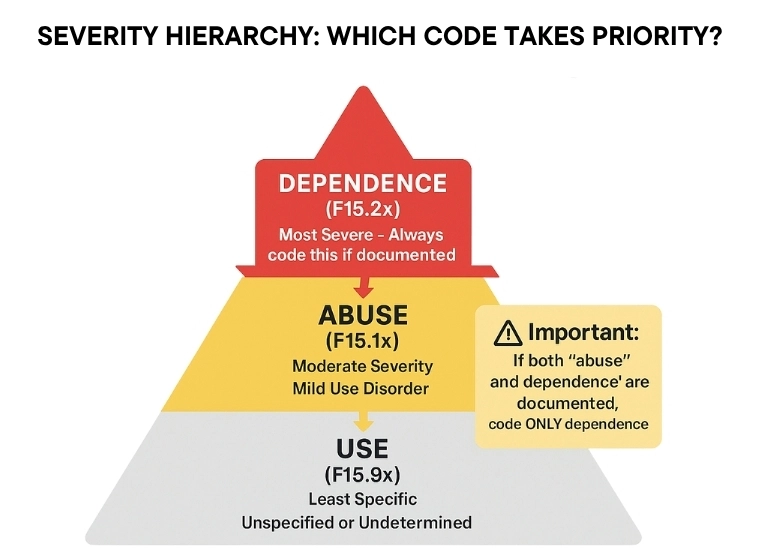
This means precision in your language matters. If you write "methamphetamine abuse and dependence" in the same note, the coder will assign only F15.2x (dependence). If you mean to convey that the patient has progressed from abuse to dependence, clarify the timeline: "Previously met criteria for mild use disorder (2022-2023), now meets criteria for severe stimulant use disorder."
Documenting Complications: Beyond the Basic Codes
Methamphetamine use rarely exists in isolation. Your patients likely present with complications and your documentation needs to capture these relationships explicitly.
Acute Presentations
F15.12/F15.22 – With Intoxication
When a patient presents with acute methamphetamine intoxication—sympathomimetic toxidrome, agitation, psychosis, don't just code uncomplicated use disorder. Document the intoxication state specifically: "Methamphetamine intoxication with psychosis" allows coding of F15.122 (abuse with intoxication and psychosis) or F15.222 (dependence with intoxication and psychosis).
F15.23 – With Withdrawal
Stimulant withdrawal often gets overlooked because it's not as dramatic as alcohol or benzodiazepine withdrawal, but it's clinically significant when your patient is experiencing the crash profound fatigue, depression, increased appetite, and anhedonia, document "stimulant withdrawal" to support F15.23 coding.
Clinical Documentation: The Seven Essential Elements
What separates adequate documentation from documentation that truly serves your patient and supports accurate coding:
1. Name the Substance Specifically
Never write "stimulant use disorder" or "illicit drug use" when you mean methamphetamine. Specificity matters for epidemiology, treatment planning, and coding accuracy.
2. Identify the Disorder Type
Choose one: use, abuse (mild disorder), or dependence (moderate/severe disorder). Better yet, use DSM-5 language with severity: "severe methamphetamine use disorder."
3. Document the Evidence
Which DSM-5 criteria does the patient meet? You don't need all 11, but documenting 4-5 key criteria for a moderate/severe diagnosis strengthens your note: "Meets 6 of 11 criteria, including tolerance, withdrawal, unsuccessful quit attempts, continued use despite knowing it exacerbates his cardiomyopathy, and spending excessive time obtaining and using."
4. Clarify Current Status
Is the patient actively using or in remission? If in remission, specify early (3-12 months) or sustained (12+ months). Include the last use date when relevant: "Last methamphetamine use: 18 months ago."
5. Document Complications
Any medical or psychiatric sequelae? Cardiomyopathy, dental decay, skin infections from injection use, cognitive impairment, psychosis, mood symptoms? Document these with clear causal relationships to methamphetamine use.
6. Record Treatment and Response
What interventions are you providing? Behavioral therapy, referral to addiction psychiatry, MAT considerations (while there's no FDA-approved medication for methamphetamine use disorder, you might be using contingency management or medications for co-occurring conditions). Document the patient's engagement, adherence, and any barriers to treatment.
7. Capture the Context
Social determinants matter. Is the patient homeless? Unemployed due to substance use? These contextual factors can be coded (e.g., Z59.0 for homelessness) and help paint the full clinical picture.
The "History of Methamphetamine Abuse ICD-10
This is where I see the most confusion in documentation. Here's the key principle: Don't just write "history of methamphetamine abuse" without context.
When to Use Remission Codes
If your patient previously met criteria for methamphetamine use disorder and is now abstinent, document it as a current condition in remission, not just as historical information. The ICD-10 guidance actually directs "history of drug dependence" to F15.21 (dependence in remission).
Document this way: "Methamphetamine dependence, in sustained remission since 2021. Patient reports no use for 3.5 years, actively engaged in NA, denies cravings."
Not this way: "PMH: meth abuse"
The remission code acknowledges that this is a chronic condition requiring ongoing monitoring, not a resolved past issue.
When to Use Personal History Codes
If the patient's methamphetamine use never reached the threshold of a disorder, perhaps they experimented in their youth but never became dependent, you might use Z86.59 (Personal history of other mental and behavioral disorders) if it's clinically relevant.
However, use this sparingly. If there were a true diagnosed disorder, the remission codes are more appropriate and informative.
Medical Necessity and Payer Considerations
Your documentation doesn't exist in a vacuum. It affects authorization for treatment, risk adjustment, and reimbursement.
Supporting Treatment Authorization
When referring for addiction treatment, whether detox, residential rehab, or intensive outpatient, insurers need to see documentation that justifies the level of care. This means:
-
Clear diagnosis with severity
-
Failed lower levels of care (if applicable)
-
Evidence of functional impairment
-
Medical or psychiatric complications
-
Risk factors requiring higher level of care
Document comprehensively: "Severe methamphetamine use disorder with methamphetamine-induced psychosis. Patient has failed two attempts at outpatient treatment, currently homeless, unable to maintain abstinence in unstructured setting. Recommend residential treatment."
Risk Adjustment and HCC Coding
In Medicare Advantage and other risk-adjusted models, F15.20 (stimulant dependence) contributes to the patient's risk score. This reflects the reality that these patients have higher healthcare utilization and complexity.
Code accurately, not opportunistically. If the patient is truly in sustained remission, code it that way, don't maintain an active dependence code to inflate risk scores. Auditors will look for documentation that supports the coded diagnosis.
Words By Author
The ICD-10 codes for methamphetamine use, whether F15.10 for abuse, F15.20 for dependence, F15.21 for remission, or the more specific codes for complications, are tools that help you tell your patient's clinical story accurately.
Take the extra minute to be specific about severity, document the criteria met, clarify whether the condition is active or in remission, and explicitly link any complications to methamphetamine use. Your documentation quality directly impacts your patient's care trajectories.
ABOUT AUTHOR

Alexander White
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.