Lung nodules can be tricky to code correctly. These small spots on chest imaging pop up frequently in radiology reports, and getting the coding right is essential for proper reimbursement and accurate patient documentation.
Here's the thing about lung nodules: they're usually incidental findings rather than definitive diagnoses. A patient comes in for a routine chest X-ray or CT scan, and suddenly there's a small round shadow on the image. Is it cancer? Probably not. Most lung nodules turn out to be benign. But until we know for sure, we need to code what we see on that imaging report.
As healthcare providers and coders, we already understand the clinical significance of these findings. What we need is clarity on the pulmonary nodule ICD 10 coding framework. Which code do you use for a single nodule versus multiple nodules? Does it matter if it's in the right lung or left lung? What about patients with a history of lung nodules?
This guide cuts through the confusion and gives you practical, straightforward answers to these coding questions. We'll walk through the key ICD-10 codes, provide documentation tips that will help you code with confidence.
Key ICD-10-CM Codes for Pulmonary Nodules: At-a-Glance Reference
The ICD-10-CM classification system groups lung nodules under category R91, which covers "Abnormal findings on diagnostic imaging of lung." The specific code you select depends primarily on whether the nodule is solitary or if multiple nodules are present.
|
ICD-10 Code |
Description |
When to Use |
|
R91.1 |
Solitary pulmonary nodule (coin lesion of lung) |
One single nodule visible on chest imaging, regardless of which lung or lobe. This is your go-to code for any isolated pulmonary nodule ICD 10 scenario. |
|
R91.8 |
Other nonspecific abnormal finding of lung field |
Multiple lung nodules, or other lung lesions that don't fit the solitary nodule definition. Also used when documentation describes an abnormal finding without clear characterization. |
|
R91.9 |
Unspecified abnormal finding of lung field |
Avoid this code whenever possible. It's non-billable and non-specific. Always try to determine if the finding is solitary or multiple to use R91.1 or R91.8 instead. |
|
Z87.09 |
Personal history of other diseases of the respiratory system |
Used when documenting a previously found lung nodule that has resolved, been removed, or is no longer present. This is the closest thing to a history of lung nodule ICD 10 code. |
R91.1: Coding Solitary Pulmonary Nodules
R91.1 is the workhorse code for lung nodule documentation. The official descriptor reads "Solitary pulmonary nodule," and it includes the synonym "coin lesion, lung." That old-fashioned term "coin lesion" comes from the fact that a solitary nodule on a chest X-ray often looks like someone dropped a coin inside the lung. A small, round, well-defined shadow.
The ICD-10 R91.1 is used when a distinct nodule is identified on imaging. It doesn't matter if that nodule is in the right upper lobe, left lower lobe, or anywhere else in either lung. There's just one of them, and that's what makes it "solitary."
Clinical Scenarios for R91.1
Scenario 1: A 58-year-old patient undergoes a chest CT for persistent cough. The radiologist reports: "8 mm nodule in the right upper lobe, smooth borders, no calcification. Recommend follow-up CT in 3 months." You would code this as R91.1.
Scenario 2: During a preoperative chest X-ray, a 1.2 cm nodule is incidentally discovered in the left lower lobe. The patient has no respiratory symptoms. The finding is described as a "coin lesion." This gets coded as R91.1.
Scenario 3: A patient with prior smoking history has screening low-dose CT that reveals a 6 mm ground-glass nodule in the right middle lobe. Until further evaluation determines what this is, you code R91.1.
Important Documentation Tips for R91.1
To support your use of R91.1, make sure the medical record includes:
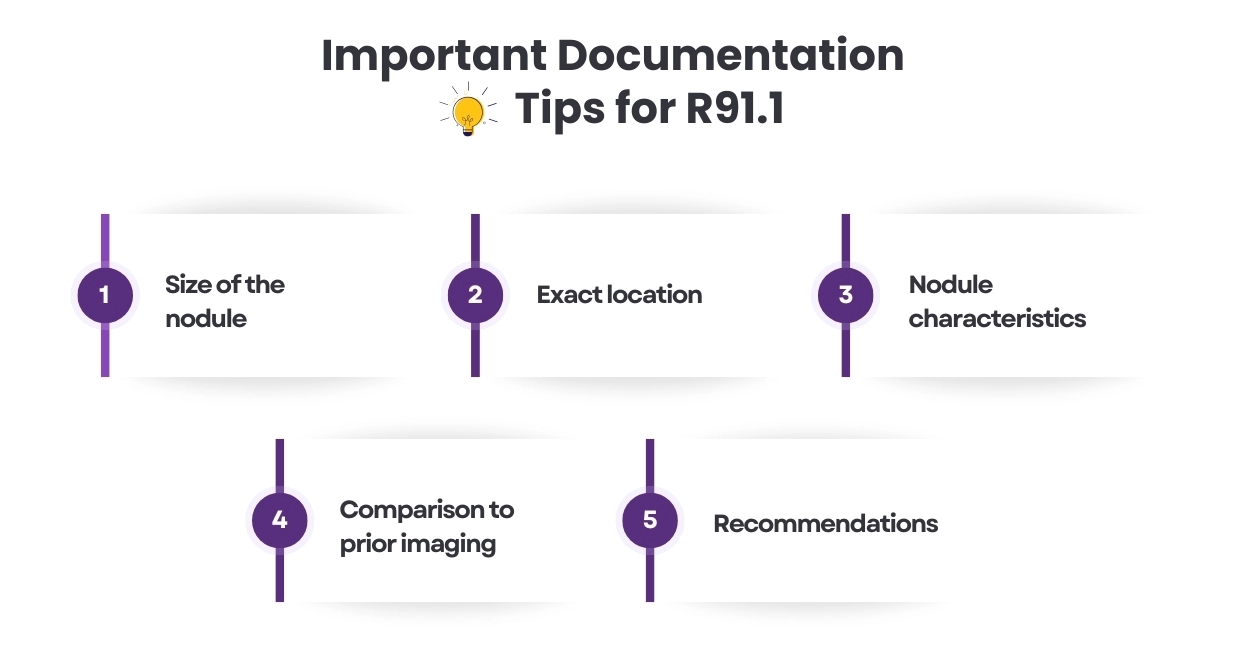
Size of the nodule: Document in millimeters or centimeters. This matters clinically for determining follow-up intervals and also supports medical necessity for surveillance imaging.
Exact location: Specify which lung (right or left) and which lobe (upper, middle, lower). While this doesn't change the ICD-10 code itself, it's essential clinical information.
Nodule characteristics: Note if it's solid, ground-glass, part-solid, calcified, spiculated, or smooth-bordered. These descriptors help assess malignancy risk.
Comparison to prior imaging: If available, document whether this is a new nodule, stable nodule, or growing nodule. Changes over time significantly impact clinical management.
Recommendations: Include the radiologist's recommendations (follow-up imaging, PET scan, biopsy, etc.). This supports medical necessity for subsequent procedures.
When NOT to Use R91.1
Stop using R91.1 once you have a definitive diagnosis. If a biopsy confirms the nodule is adenocarcinoma of the lung, you switch to coding the specific lung cancer diagnosis. If pathology shows it's a hamartoma (benign tumor), you code that instead. The solitary nodule of lung ICD 10 code is a placeholder for "we found something on imaging that needs investigation," not a final diagnosis.
Also, don't use R91.1 if there are multiple nodules. That single word "solitary" is critical,it means one and only one. If the radiology report describes "scattered nodules" or "multiple nodules," you need a different code, which we'll cover next.
R91.8: Coding Multiple Nodules and Other Lung Findings
R91.8 carries the descriptor "Other nonspecific abnormal finding of lung field." This code serves as the catch-all for lung imaging abnormalities that don't fit the solitary nodule category. Most commonly, coders use R91.8 for multiple pulmonary nodules.
Think of it this way: R91.1 is for "one nodule," and R91.8 is for "more than one nodule or other weird stuff we're seeing on the scan."
When to Assign R91.8
Use Case 1: Multiple Pulmonary Nodules
The most straightforward application of R91.8 is when imaging reveals more than one nodule. If a CT scan reports "multiple bilateral pulmonary nodules," you assign R91.8. It doesn't matter if there are two nodules, five nodules, or dozens. If the count is greater than one, R91.8 is your code.
Use Case 2: Unspecified or Unclear Findings
Sometimes radiology reports are frustratingly vague. You might see language like "abnormal opacity in the right lung" or "possible lesion versus artifact" without clear specification of whether it's a true nodule. In these cases, R91.8 serves as the lung lesion ICD 10 code when the finding doesn't meet the clean definition of a solitary nodule.
Use Case 3: Multiple Nodules with One Dominant Lesion
Here's a nuance worth knowing: sometimes a patient has multiple small nodules but one significantly larger or more concerning nodule. According to CMS guidance, you still use R91.8 in this scenario because multiple nodules are present, even though clinical attention may focus on the dominant one.
Documentation Best Practices for R91.8
When coding multiple nodules, strengthen your documentation by including:
Number of nodules: If the radiologist counts them, document that number. "Three nodules" or "innumerable small nodules" tells a story.
Size range: Note the size of the largest nodule and smallest if mentioned. "Multiple nodules ranging from 3 mm to 12 mm" is helpful.
Distribution pattern: Are they throughout both lungs (bilateral), confined to one lung (unilateral), upper lobes, lower lobes? This matters clinically.
Character of nodules: Are they all calcified (suggesting benign granulomas)? Are some solid and others ground-glass? Mixed patterns have different implications.
Clinical context: If these nodules are being evaluated as possible metastases in a patient with known cancer elsewhere, document that. It explains the clinical reasoning for workup.
The R91.8 vs. R91.9 Distinction
You might wonder about R91.9, which is designated "Unspecified abnormal finding of lung field." Here's the deal: R91.9 is non-billable and should be avoided whenever possible. It's too vague and most payers will reject it.
If you're tempted to use R91.9 because documentation is unclear, try to push for R91.8 instead.
Think of R91.8 as "specified-but-not-fitting-other-categories" while R91.9 is "we literally have no idea what this is."
In practical coding, when you need an ICD 10 code for lung nodule unspecified because documentation doesn't clarify solitary versus multiple, default to R91.8 rather than falling back to R91.9.
The Laterality Question: Right Lung Nodule vs. Left Lung Nodule Coding
Here's something that trips up coders all the time: Does the side matter when coding lung nodules? Do I need different codes for a right lung nodule ICD 10 versus a left lung nodule ICD 10?
The short answer: No, there are no laterality-specific codes for lung nodules in ICD-10-CM.
Why Laterality Doesn't Change the Code
Both R91.1 and R91.8 inherently cover nodules in any location within the lungs. Unlike some ICD-10 diagnoses that have distinct codes for right versus left (think about how fracture codes often specify which side), the lung nodule codes don't make this distinction.
A solitary nodule in the right lung gets coded as R91.1. A solitary nodule in the left lung also gets coded as R91.1. The code is the same.
But You Still Need to Document the Side
Now, don't misunderstand just because the ICD-10 code doesn't change based on laterality doesn't mean you shouldn't document which lung is involved. You absolutely should. Here's why:
Clinical necessity: The exact location matters for follow-up imaging, biopsy planning, and surgical approaches if needed.
Complete documentation: Medical records should paint a complete clinical picture. "Solitary nodule, right upper lobe" is better documentation than just "lung nodule."
Justification for procedures: If a patient needs a right-sided thoracoscopy, the documentation should clearly state the nodule is on the right side, even though the diagnosis code doesn't reflect that.
Tracking and surveillance: For patients with multiple nodules over time or nodules in different locations at different encounters, specifying location helps track each individual finding.
Proper documentation example:
"Finding: Solitary pulmonary nodule, right upper lobe, measuring 9 mm with smooth margins.
ICD-10 Code: R91.1"
Another example:
"Finding: Two nodules identified 6 mm nodule in left upper lobe and 4 mm nodule in right lower lobe.
ICD-10 Code: R91.8"
Notice how the documentation specifies exactly where each nodule is located, but the code selection is based solely on whether we're dealing with one nodule or multiple nodules.
Coding History of Lung Nodules
What happens when you're documenting a patient who had a lung nodule in the past, but it's no longer there? Maybe it was surgically removed, maybe it resolved on its own, or maybe follow-up imaging showed it completely disappeared. How do you code that historical finding?
No Specific History Code
ICD-10-CM doesn't provide a dedicated code that says "personal history of lung nodule." We have to work with what's available in the coding system, which means using a broader category code.
Z87.09: Your Best Option
Z87.09 is designated as "Personal history of other diseases of the respiratory system." This is a catch-all code for past respiratory conditions that don't have their own specific history codes. It's your go-to option for coding history of lung nodule ICD 10 scenarios.
When to Use Z87.09
Use this code when:
A nodule was previously documented but is no longer present: Follow-up imaging shows complete resolution, or surgical resection removed it.
The historical nodule is relevant to current care: You're mentioning the prior nodule because it influences current clinical decision-making or explains why the patient is on a surveillance imaging protocol.
No current acute lung findings: The patient doesn't have an active nodule right now; you're just documenting their past medical history.
Example scenario: A patient had a 10 mm nodule three years ago that was monitored with serial CT scans. The nodule shrank over time and disappeared completely. Now the patient is seeing you for an annual physical, and you note in their PMH: "History of resolved pulmonary nodule." You would code Z87.09 as a secondary diagnosis.
Important Limitations of Z87.09
Remember that Z codes are supplementary. They provide context but shouldn't be your principal diagnosis for an encounter. You use Z87.09 in addition to whatever else is going on clinically.
Also, if that prior nodule turned out to be something specific, use the more specific history code instead. For example:
If the nodule was lung cancer: Use Z85.118 (Personal history of other malignant neoplasm of bronchus and lung) rather than Z87.09.
If the nodule was due to TB: Consider Z86.11 (Personal history of tuberculosis) if that's the relevant historical diagnosis.
If it was truly just a benign, indeterminate nodule that resolved: Z87.09 is perfect.
Documentation Best Practices for Lung Nodule Coding
Good coding starts with good documentation. Here's what you need in the medical record to support accurate pulmonary nodule ICD 10 code assignment.
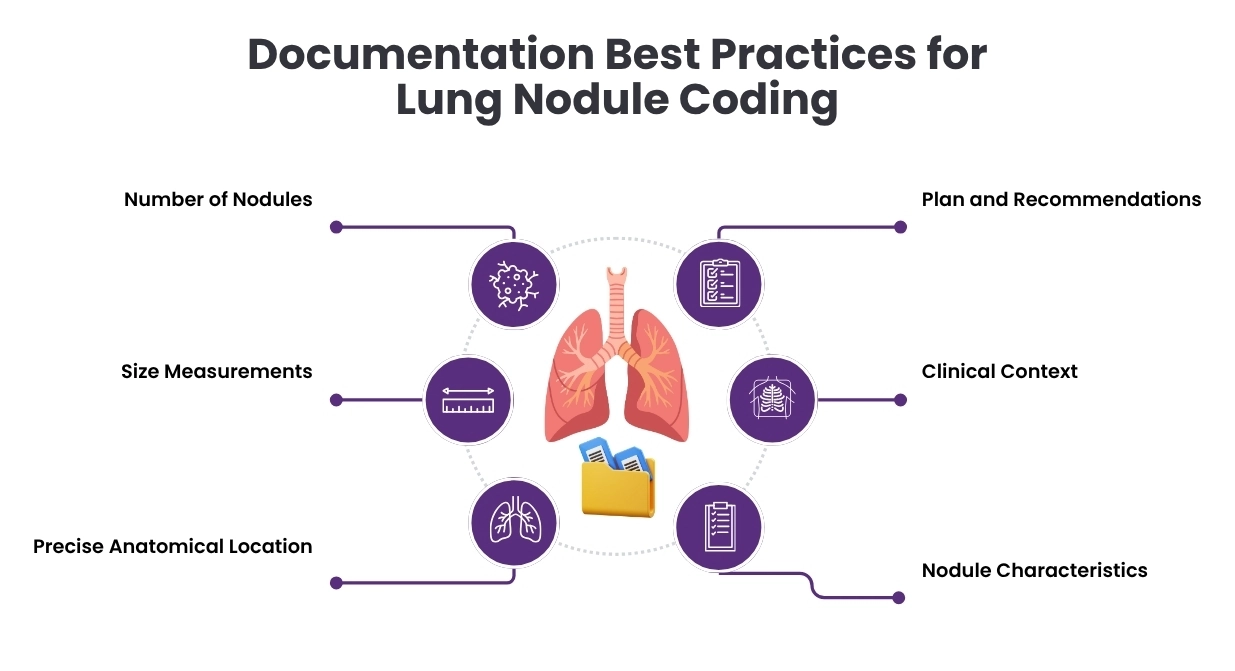
Essential Elements to Document
1. Number of Nodules
State clearly whether imaging shows one nodule, multiple nodules, or if the number is uncertain. Use specific language:
-
"Solitary nodule"
-
"Two nodules identified"
-
"Multiple scattered nodules"
-
"Innumerable small nodules"
This single piece of information determines whether you're coding R91.1 or R91.8.
2. Size Measurements
Always document size in millimeters or centimeters. Include:
-
Longest diameter for each nodule
-
If multiple nodules, at least note the size of the largest
-
Comparison to prior imaging if available ("stable at 8 mm" or "increased from 6 mm to 9 mm")
3. Precise Anatomical Location
Specify:
-
Which lung (right or left)
-
Which lobe (upper, middle, lower)
-
Specific segment if mentioned by radiologist
Example: "Right upper lobe, apical segment" is better than just "right lung."
4. Nodule Characteristics
Include descriptive details:
-
Solid, ground-glass, or part-solid
-
Margins (smooth, spiculated, lobulated, irregular)
-
Calcification pattern (central, popcorn, laminated, eccentric, or none)
-
Cavitation if present
These characteristics help assess malignancy risk and justify follow-up intensity.
5. Clinical Context
Explain why this finding matters:
-
Incidental finding during unrelated imaging
-
Found on screening CT in high-risk patient
-
New finding in patient with known cancer
-
Being monitored due to growth on prior imaging
6. Plan and Recommendations
Document what happens next:
-
Follow-up CT in 3 months, 6 months, 12 months
-
PET scan ordered to assess metabolic activity
-
Referral to pulmonology for bronchoscopy
-
Referral to thoracic surgery for biopsy
This supports medical necessity for subsequent procedures and visits.
Language That Supports Clear Coding
Use specific terminology that makes coding decisions obvious:
Good documentation: "Solitary 8 mm nodule right upper lobe" → clearly R91.1
Good documentation: "Three nodules identified in bilateral upper lobes" → clearly R91.8
Problem documentation: "Lung lesion noted" → is it one or more? Need clarification.
Problem documentation: "Abnormal chest X-ray" → too vague, what's abnormal?
When you use precise language, you make the coder's job easier and reduce the need for queries.
Avoiding Common Documentation Pitfalls
Pitfall 1: Copying forward old imaging findings without verifying current status.
Solution: Always base coding on the most recent imaging report for the current encounter.
Pitfall 2: Using terminology inconsistently (calling it a "nodule" in one note and "mass" in another).
Solution: Use consistent, accurate terminology. If it's less than 3 cm, it's a nodule. If it's 3 cm or larger, call it a mass.
Pitfall 3: Not documenting follow-up plans.
Solution: Even if the radiologist makes recommendations in their report, the ordering provider should document the plan in their note (agree with recs, will order follow-up, discussed with patient, etc.).
Pitfall 4: Failing to document when nodules resolve.
Solution: If follow-up imaging shows a previously documented nodule is gone, clearly state this. It supports stopping surveillance and potentially adding Z87.09 to document the history.
Special Considerations for Screening and Surveillance
Lung nodule coding gets more complex when you're dealing with screening programs and surveillance imaging. Here's what you need to know.
Lung Cancer Screening Context
The United States Preventive Services Task Force (USPSTF) recommends annual low-dose CT screening for lung cancer in adults aged 50 to 80 years who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years.
Initial screening visit coding:
-
Primary diagnosis: Z12.2 (Encounter for screening for malignant neoplasm of respiratory organs)
-
Risk factors: F17.210 (current smoker) or Z87.891 (former smoker)
-
This applies when NO nodules are found on the screening CT
Screening that identifies a nodule:
-
Primary diagnosis: R91.1 (if solitary nodule found) or R91.8 (if multiple nodules found)
-
Secondary diagnosis: Z12.2 can still be included to show this was a screening encounter
-
Risk factors: Include tobacco codes
Subsequent surveillance imaging: Once a nodule is found, follow-up CTs are no longer "screening",they're diagnostic surveillance. The primary diagnosis for these encounters should be R91.1 or R91.8, not Z12.2.
Integrating ICD-10 Coding with CPT Procedures
Understanding the relationship between diagnosis codes and procedure codes helps ensure complete and accurate billing.
Common Procedures Related to Lung Nodule Evaluation
Imaging Studies:
-
71250: CT chest without contrast
-
71260: CT chest with contrast
-
71270: CT chest without and with contrast
-
71045-71048: Chest X-ray (various views)
-
78811-78816: PET scan codes
When billing these procedures for nodule evaluation, R91.1 or R91.8 serves as the diagnosis code supporting medical necessity.
Biopsy Procedures:
-
32405: Bronchoscopy with biopsy
-
32554: Thoracentesis
-
32606: Transbronchial lung biopsy
-
32607: Endobronchial ultrasound with biopsy
For biopsy procedures, R91.1 or R91.8 is appropriate if no definitive diagnosis exists yet. Once pathology confirms a diagnosis, update coding accordingly.
Surgical Procedures:
-
32480: Removal of lung, total pneumonectomy
-
32663: Thoracoscopy with lobectomy
-
32666: Thoracoscopy with wedge resection
For surgical resection, you might code R91.1 preoperatively, but postoperative coding should reflect the surgical pathology diagnosis.
Linking Diagnoses to Procedures
Medicare and most payers require appropriate linkage between diagnosis codes and procedure codes. When a patient undergoes a CT chest for nodule follow-up, the claim should show:
Procedure: 71250 (CT chest without contrast) Linked diagnosis: R91.1 (solitary pulmonary nodule)
This linkage demonstrates that the procedure was medically necessary based on the documented diagnosis.
Payer-Specific Considerations and Requirements
Different insurance payers have varying requirements for lung nodule coding and coverage.
Medicare Guidelines
Medicare has specific Local Coverage Determinations (LCDs) for imaging and procedures related to lung nodules:
PET scan coverage: Medicare typically covers PET scans for characterization of solitary pulmonary nodules when:
-
Nodule is larger than 8 mm
-
Conventional imaging is indeterminate
-
There's no extrathoracic metastatic disease
R91.1 would be the diagnosis supporting PET scan medical necessity in this scenario.
CT screening coverage: Medicare covers annual lung cancer screening with LDCT for beneficiaries who meet specific criteria. Initial visits require shared decision-making documentation and tobacco cessation counseling.
Commercial Payer Variations
Commercial insurers may have different policies:
Prior authorization: Some payers require prior auth for repeat CT scans within certain timeframes. Your coding and documentation must justify the medical necessity.
Frequency limitations: Payers may limit how often surveillance imaging can be performed. Documentation must show adherence to clinical guidelines.
Multiple nodule scenarios: When coding R91.8 for multiple nodules, some payers may require specific documentation about which nodule is being followed or whether all are being monitored.
Documentation to Support Coverage
Regardless of payer, strengthen your coding with documentation that includes:
-
Clinical indication for imaging
-
Patient risk factors
-
Rationale for imaging frequency
-
Reference to clinical guidelines (Fleischner, Lung-RADS, NCCN)
-
Interval change documentation
-
Plan based on findings
Words By Author
Coding lung nodules correctly comes down to understanding a few key principles and applying them consistently. The pulmonary nodule ICD 10 framework is straightforward once you grasp the basic rules: one nodule gets R91.1, multiple nodules get R91.8, and laterality doesn't change the code.
Lung nodule coding represents just one of many complex scenarios in medical billing and coding. When you need expertise you can trust, HMS USA LLC delivers comprehensive coding solutions tailored to your healthcare organization's needs.
Our team of certified professional coders specializes in radiology coding, pulmonary coding, and oncology coding with deep expertise in conditions like lung nodules, pulmonary masses, and respiratory abnormalities. We understand the nuances that distinguish R91.1 from R91.8, know when to query providers for clarification, and stay current with evolving payer requirements.
ABOUT AUTHOR

Alexander White
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.