Have you ever had a patient ask, “Can I just pay you directly?” Or wondered about the rules when someone with insurance or even Medicare or Medicaid wants to self-pay? Here’s what every healthcare provider should know about self-pay in medical billing, from legal considerations to best practices and common self-pay medical services.
What is Self-Pay in Medical Billing?
Self-pay in medical billing refers to situations where the patient pays for their healthcare services out-of-pocket, rather than using health insurance or any third-party payer. This can happen for two main reasons:
-
The patient is uninsured (has no coverage).
-
The patient is insured, but chooses not to use their insurance for a particular visit or procedure.
In both cases, the patient is responsible for the full cost of care. Self-pay is more common than many providers realize, and it comes with specific legal and practical considerations.
Is it Legal to Self-Pay When You Have Insurance?
Yes, it is legal to self-pay even when you have insurance, but with some important caveats.
For Private (Commercial) Insurance:
Patients have the right to self-pay for a service instead of using their insurance, whether for privacy, convenience or to obtain a service not covered by their plan. Federal law (HIPAA) supports this right. If a patient pays in full and requests the provider not to bill their insurance, the provider must comply.
However, providers should check their contracts with insurers. Some insurance contracts restrict in-network providers from accepting cash payments for covered services without submitting a claim.
Practical Tip:
If your patient asks to self-pay, have them sign a short agreement acknowledging their financial responsibility and their request not to submit an insurance claim.
When Can a Medicare Patient Legally Self-Pay?
There are a few, very specific circumstances where self-pay is allowed for Medicare beneficiaries:
1. Services NOT Covered by Medicare
-
Examples: Cosmetic surgery, most routine dental or vision care, hearing aids, “wellness” or preventive therapies not deemed medically necessary.
-
In these situations, Medicare is not involved, so you can charge the patient directly.
-
Best practice: Always inform the patient in advance and have them sign a simple notice acknowledging that the service isn’t covered by Medicare and they will pay out-of-pocket.
2. Services That Might Not Be Covered (Use of an Advance Beneficiary Notice (ABN)
-
If you suspect a normally covered service may not be considered medically necessary for this patient (for instance, a test or therapy that exceeds Medicare’s frequency limits), use an Advance Beneficiary Notice (ABN).
-
With an ABN, the patient is informed Medicare may not pay, and they can choose to proceed and pay out-of-pocket if denied.
-
Under ABN “Option 2,” the patient can even request that you don’t submit a claim to Medicare at all.
-
Important: ABNs can’t be used to bypass Medicare for services that are medically necessary and typically covered. They’re only for cases where coverage is uncertain.
3. Seeing a Provider Who Has Opted Out of Medicare (Private Contract)
-
Some providers (e.g., certain primary care doctors, psychiatrists) may formally opt out of Medicare. This means:
-
They’ve notified Medicare and signed an affidavit for a two-year period.
-
They must have every Medicare patient sign a private contract stating Medicare won’t be billed and the patient will pay entirely out-of-pocket.
-
-
In this opt-out scenario, the provider sets their own rates and Medicare is not involved in the billing or reimbursement at all.
Note: Not all provider types are eligible to opt out.
4. Incidental/Statutorily Non-Covered Services
Some items and services are specifically excluded from Medicare by law (for instance, routine foot care, hearing aids, most chiropractic services beyond spine manipulation).
No ABN is required, but it’s wise to notify patients in writing.
What If a Medicare Patient Just Wants to Pay Cash?
If the patient says, “Can’t I just pay you cash and not involve Medicare?” Unless one of the above exceptions applies, you must say no.
-
If you’re enrolled in Medicare and the service is covered, federal law requires you to bill Medicare.
-
Providers who have NOT opted out of Medicare cannot accept full payment in cash for covered services.
-
This protects patients from overpaying and helps Medicare track utilization and costs.
Rules for Charging Self-Pay Patients
To keep your practice compliant and patient-friendly, follow these best practices and federal requirements:
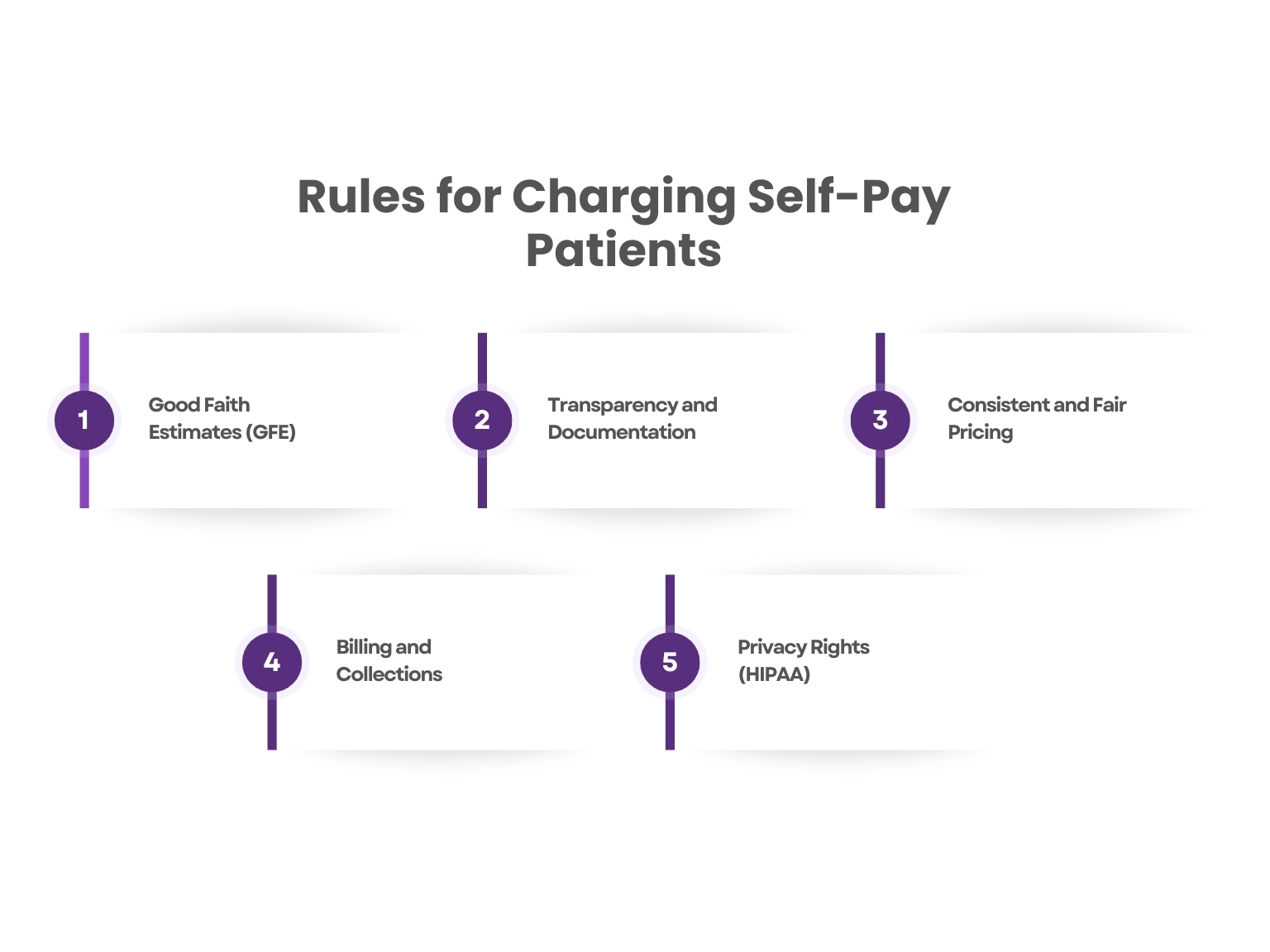
1. Good Faith Estimates (GFE)
-
Required by law under the No Surprises Act for uninsured or self-pay patients.
-
Provide an itemized estimate of charges before treatment (at least 1 business day in advance for scheduled services).
2. Transparency and Documentation
-
Disclose full charges and payment terms before service is rendered.
-
Use a simple consent form or “self-pay agreement”—especially if the patient is insured but opts not to use their coverage.
3. Consistent and Fair Pricing
-
Avoid charging self-pay patients excessively more than you charge insured patients. Many practices offer discounted rates for self-pay to reflect what insurance typically pays.
4. Billing and Collections
-
Be upfront about payment plans or financial assistance for those who need it.
-
Provide an itemized bill and clear contact information for billing questions or disputes.
5. Privacy Rights (HIPAA)
-
If an insured patient self-pays and asks you not to share the info with their plan, you must comply—don’t submit the claim or disclose the visit.
What Is a Medicaid Self-Pay Agreement?
A Medicaid Self-Pay Agreement is a written document that a provider uses when a Medicaid patient agrees to pay out-of-pocket for services that Medicaid does not cover or when the patient wants services beyond Medicaid’s coverage limits.
Because Medicaid forbids “balance billing” patients for covered services, providers must be transparent and obtain informed consent when charging patients privately for non-covered services.
When Do You Need a Medicaid Self-Pay Agreement?
-
Non-Covered Services:
Medicaid does not cover every healthcare service. Examples include certain elective procedures, some dental or vision services, or therapies exceeding Medicaid limits. When providing these non-covered services, the provider should:-
Inform the patient the service is not covered by Medicaid.
-
Obtain the patient’s agreement to pay privately before the service is performed.
-
-
Services Beyond Medicaid Limits:
Medicaid plans often limit the number or frequency of certain services, like physical therapy visits. If a patient wants additional sessions beyond those limits, the provider can offer a self-pay option with a signed agreement. -
Patients Seeing Non-Medicaid Providers:
If a Medicaid beneficiary chooses a provider who is not enrolled in Medicaid, the provider treats them as a self-pay patient. In this case, a self-pay agreement clarifies the patient’s financial responsibility upfront.
Words By Author
Understanding the ins and outs of self-pay in medical billing is essential for every healthcare provider today. Whether dealing with uninsured patients, privately insured individuals choosing to pay out-of-pocket, or navigating the complex rules around Medicare and Medicaid, clear communication and compliance are key.
Always provide accurate cost estimates, obtain proper patient consent, and follow federal and state regulations to protect both your practice and your patients. By staying informed and proactive, you can ensure a smooth billing experience that builds trust and avoids surprises. If you haven’t already, consider developing standardized self-pay agreements and training your team on best practices—small steps that make a big difference.
ABOUT AUTHOR

John Wick
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.