Hands-on healing is your specialty, but translating those skilled manual therapy techniques into accurate reimbursement? That's where things can get tricky. If you've ever felt uncertain about billing for manual therapy or wondered if you're coding accurately for the techniques involved, this guide is a must-read.
What is CPT Code 97140?
CPT code 97140 is a billing code used to report manual therapy techniques performed by qualified healthcare professionals. This code covers explicitly a variety of hands-on treatments that aim to improve function, reduce pain, and enhance mobility. Understanding the specific parameters of this code is essential to ensure accurate billing and optimal reimbursement.
Understanding the Time-Based Billing Rules for 97140
Unlike some CPT codes that are billed per service, CPT code 97140 operates on a time-based system. This means that the duration of the manual therapy session directly determines the number of units you can bill.
Medicare follows the 8-minute rule for time-based codes like 97140. This means that in order to bill a unit, at least 8 minutes of that 15-minute increment must be spent providing direct patient contact. Any time less than 8 minutes within an increment cannot be counted towards billing.
Billing in 15-Minute Increments
Each unit of CPT code 97140 represents 15 minutes of direct, one-on-one patient contact during which the therapist is performing skilled manual therapy techniques. These 15-minute increments are non-cumulative, meaning you can only bill for full units, not fractions.
-
Example 1: A 20-minute manual therapy session would be billed as one unit of 97140.
-
Example 2: A 40-minute session would be billed as two units of 97140.
Billing for Multiple Body Regions
If you perform manual therapy on multiple body regions during a single session, you can still bill 97140, but the direct contact time for each region is tracked separately. The total billable units are determined by adding up the time spent on each region and converting it into 15-minute increments.
Example: 15 minutes of manual therapy on the neck, 10 minutes on the low back, and 20 minutes on the shoulder would be billed as two units of 97140 (15 + 10 + 20 = 45 minutes = 3 units, but since one unit is under 15 minutes it can't be billed).
Does CPT Code 97140 Require to Use of Modifiers?
CPT code 97140 may require the use of modifiers in certain situations to provide additional information to payers and ensure accurate reimbursement. Here are some common modifiers used with 97140 and when to apply them:
Always Therapy Modifiers:
-
GP: This modifier indicates that the services were provided by a physical therapist. It's required for Medicare claims and often used by other payers as well.
-
GO: This modifier is used when the services are provided by an occupational therapist.
Therapy Cap Modifiers:
-
KX: This modifier is used when the services exceed the Medicare therapy cap but are still medically necessary. It indicates that the provider has determined that the services are reasonable and necessary for the patient's condition.
Other Modifiers:
-
59: This modifier may be used when 97140 is performed in a separate and distinct 15-minute increment from other manual therapy codes or procedures during the same session. It's important to note that this modifier has specific rules and should only be used when appropriate.
-
97: This modifier can be used to indicate that manual lymphatic drainage was a component of the manual therapy services provided.
Who Can Bill For CPT Code 97140?
Not just anyone can bill for CPT code 97140. It's reserved for qualified healthcare professionals who have the appropriate training, licensure, and expertise in performing manual therapy techniques. Here's a breakdown of who is typically eligible to bill for this code:
Qualified Healthcare Professionals:
-
Physical Therapists (PTs): PTs are often the primary providers of manual therapy services, using hands-on techniques to address musculoskeletal and neuromuscular conditions.
-
Occupational Therapists (OTs): OTs may also use manual therapy as part of their treatment plans, particularly when focusing on improving functional abilities and daily living skills.
-
Chiropractors: Chiropractors specialize in manual adjustments and manipulation of the spine and other joints, making them well-suited to bill for 97140.
-
Physicians: In some cases, physicians who have specialized training in manual therapy techniques (e.g., physiatrists, osteopathic physicians) may also be eligible to bill for this code.
Types of Manual Therapy Techniques Applicable to Bill with CPT Code 97140
CPT code 97140 encompasses a diverse range of manual therapy techniques aimed at improving function, reducing pain, and enhancing mobility. Here's a closer look at some common techniques that fall under this code:
1. Soft Tissue Mobilization/Massage:
This technique involves the skilled manipulation of muscles, tendons, ligaments, and fascia to relieve tension, reduce pain, improve circulation, and promote healing.
-
Billing: Soft tissue mobilization performed as a therapeutic intervention (not for relaxation) can be billed under 97140. It's essential to document the specific techniques used (e.g., effleurage, petrissage, trigger point release) and the treatment goals for each area.
2. Joint Mobilization/Manipulation:
These techniques involve skilled passive movements of joints to improve range of motion, reduce pain, and restore normal joint function.
-
Billing: Both joint mobilization and manipulation can be billed under 97140. Documentation should specify the type of mobilization/manipulation used (e.g., grade I-V mobilization, high-velocity low-amplitude thrust), the specific joint(s) treated, and the patient's response.
3. Lymphatic Drainage Massage:
This specialized technique involves gentle, rhythmic strokes to stimulate lymphatic flow and reduce swelling, particularly in patients with lymphedema.
-
Billing: Manual lymphatic drainage performed by a qualified therapist (e.g., certified lymphedema therapist) can be billed under 97140. Documentation should include the specific areas treated, the duration of treatment, and the patient's response.
4. Myofascial Release:
This technique focuses on releasing restrictions and tension in the fascia (the connective tissue that surrounds muscles and organs) to improve mobility, reduce pain, and restore function.
-
Billing: Myofascial release, when performed as a therapeutic intervention, can be billed under 97140. Documentation should describe the specific techniques used (e.g., skin rolling, cross-hand release) and the areas treated.
5. Stretching:
While therapeutic stretching may be part of a manual therapy session, it's typically not billed separately under 97140. It's considered a component of the overall treatment and is often included in the documentation to support the use of 97140.
-
Billing: If stretching is the sole intervention, you would not bill for 97140. However, if it's integrated with other manual therapy techniques and contributes to the overall treatment goals, it can be included in the documentation to support the use of 97140.
6. Graston Technique:
This instrument-assisted soft tissue mobilization technique uses specialized tools to detect and break down scar tissue and fascial restrictions.
-
Billing: While the Graston Technique itself is not a billable code, the manual therapy techniques performed with the instrument (e.g., soft tissue mobilization, myofascial release) can be billed under 97140. Documentation should specify that the Graston Technique was used as part of the treatment.
Medical Necessity Requirements for Documenting Manual Therapy
To successfully bill for manual therapy using CPT code 97140, it's not enough to simply perform the techniques; you must also establish and document the medical necessity of the treatment. This ensures that the services provided are appropriate, effective, and meet the standards of care for the patient's condition.
Conditions Warranting Manual Therapy (97140)
-
Cervical Radiculopathy
-
Restricted Joint Motion
-
Adjunct to Therapeutic Exercise
-
Adjunct to Other Therapies
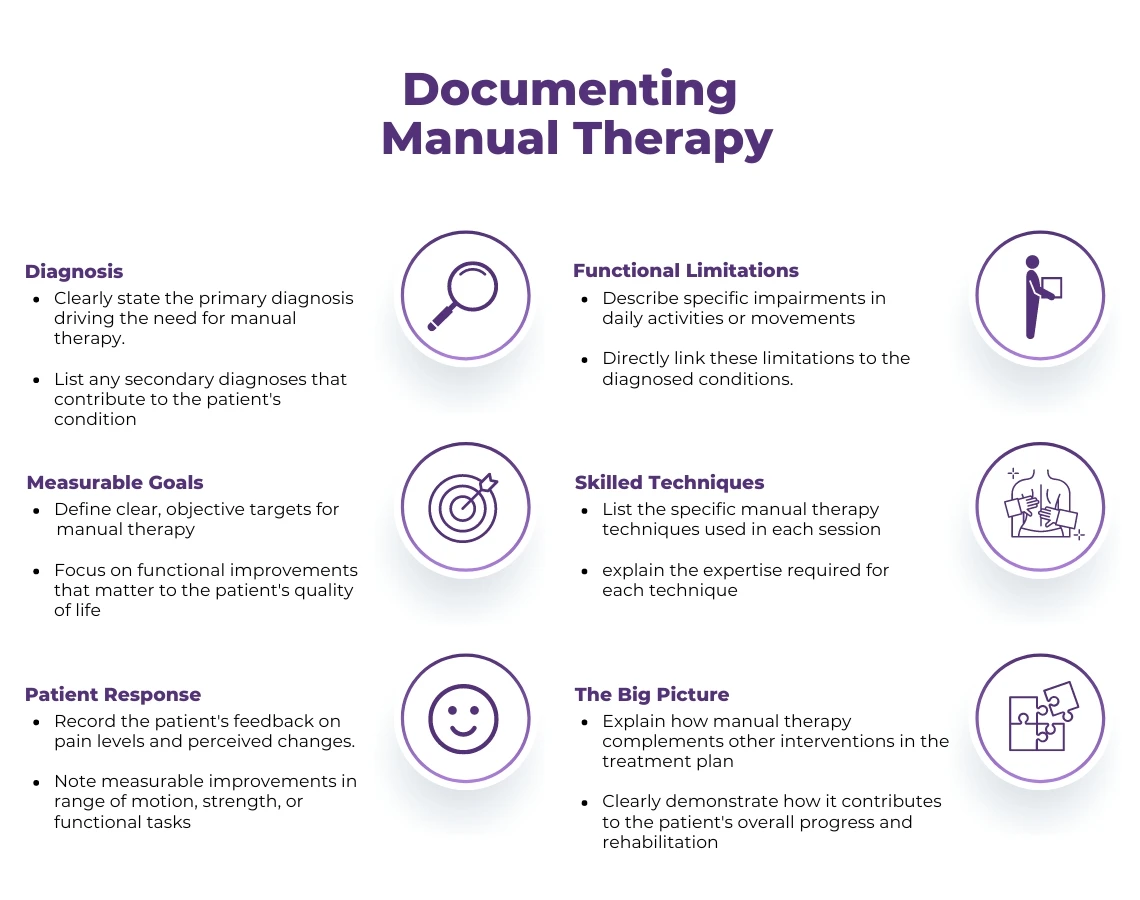
Documentation Best Practices
-
Clear Diagnosis: Clearly document the patient's primary diagnosis and any relevant secondary diagnoses that support the medical necessity of manual therapy.
-
Functional Limitations: Describe the patient's specific functional limitations (e.g., difficulty reaching overhead, limited walking distance) that are directly related to the diagnosis and can be addressed through manual therapy.
-
Treatment Goals: Establish measurable and functional goals for manual therapy, such as increased range of motion, decreased pain, or improved ability to perform specific activities.
-
Skilled Intervention: Document the specific manual therapy techniques used, emphasizing the skill and expertise required to perform them.
-
Patient Response: Note the patient's response to each manual therapy session, including changes in pain, range of motion, functional ability, and overall progress towards goals.
-
Plan of Care: Connect the manual therapy to the overall plan of care, demonstrating how it contributes to the patient's progress and rehabilitation.
ABOUT AUTHOR

John Wick
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.