Helping patients transition from hospital to home is challenging enough, and the last thing anyone needs is added stress from billing confusion. As a provider offering TCM services, you might find it tricky to bill for TCM services, especially when trying to ensure the full 30-day service period is covered and the correct codes are used for proper reimbursement.
This blog aims to clarify the process for you. We’ll dive into the specifics of when and how to use these two hospital follow-up CPT codes, explore the guidelines in detail, and discuss the reimbursement rates to help you get it right.
TCM CPT Codes
Under the Physician Fee Schedule (PFS), Medicare recognizes the importance of Transitional Care Management (TCM) and provides reimbursement for two specific CPT codes when billing for these services:
- CPT code 99495 and CPT code 99496.
These codes essentially categorize the complexity of the medical decision-making involved in each patient's TCM care plan, ensuring appropriate compensation for the level of service provided.
CPT 99495 - Comprehensive TCM Services with Moderate Medical Decision Complexity (Hospital Follow-Up within 14 Days)
When a patient requires moderate medical decision complexity during their transition from an inpatient setting (such as a hospital or skilled nursing facility) to their home or another care setting, CPT code 99495 is used. This code signifies a comprehensive array of TCM services provided within 14 days of discharge.
These services encompass:
-
Interactive contact: At least one face-to-face visit with the patient within either 7 or 14 days of discharge, depending on medical necessity.
-
Non-face-to-face services: Additional communication and care coordination activities, including phone calls, electronic communication, and interactions with other healthcare providers.
-
Medical decision-making of moderate complexity: The physician or other qualified healthcare professional assesses the patient's condition, reviews medications, coordinates care with other providers, and addresses any potential complications or barriers to recovery.
CPT 99496 - Comprehensive TCM Services with High Medical Decision Complexity (Hospital Follow-Up within 7 Days)
For patients with complex medical needs requiring high medical decision complexity during their transition, CPT code 99496 is billed. This code reflects a higher level of TCM services provided within 7 days of discharge.
The services included are similar to those under CPT 99495 but involve more intensive care coordination and medical decision-making:
-
Interactive contact: A face-to-face visit with the patient within 7 days of discharge is mandatory.
-
Non-face-to-face services: Extensive communication and care coordination efforts are undertaken to manage the patient's complex medical needs.
-
Medical decision-making of high complexity: The physician or qualified healthcare professional engages in in-depth assessment, medication management, and care coordination and addresses intricate medical issues, potential complications, and barriers to the patient's recovery.
Who Can Bill For TCM Services?
While physicians of any specialty can bill for TCM services, certain non-physician practitioners (NPPs) are also eligible to provide and bill for these services, including:
-
Clinical nurse specialists (CNSs)
-
Nurse practitioners (NPs)
-
Physician assistants (PAs)
-
Certified nurse midwives (CNMs)
It's important to note that NPPs can provide and bill for TCM services independently or "incident to" the services of a physician, depending on the specific circumstances and applicable regulations
Reimbursement Rates for TCM CPT Codes
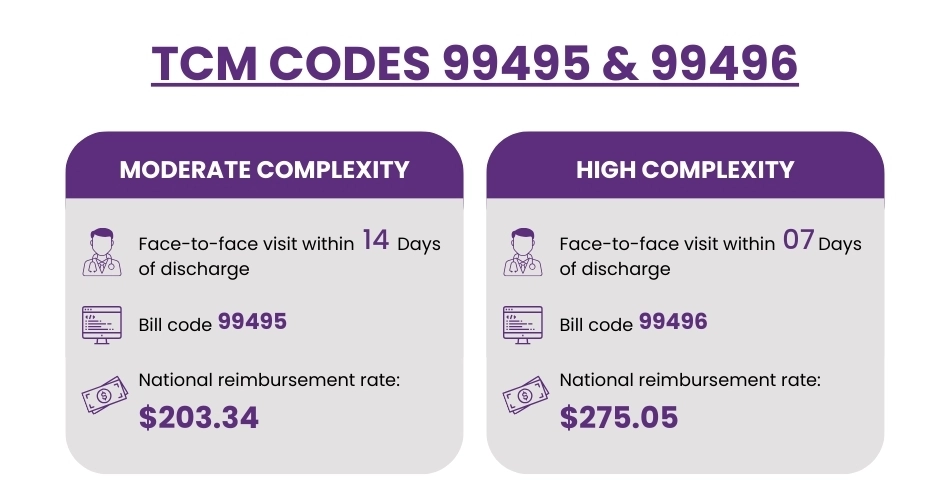
While reimbursement rates can fluctuate based on geographical location and other factors, let's look at the national average reimbursement rates for 2024 as a general guideline:
-
CPT 99495 (Moderate Medical Decision Complexity): $203.34
-
CPT 99496 (High Medical Decision Complexity): $275.05
Actual reimbursement rates can vary depending on your specific location and other factors, such as the patient's insurance plan and any contractual adjustments. It's always recommended that the specific reimbursement rates be verified with the relevant payer or that online resources like the CMS Physician Fee Schedule Search tool be utilized.
Crucial Coding Guidelines for CPT Code 99495 and 99496
To guarantee seamless billing and sidestep potential claim rejections, it's imperative to keep these crucial coding pointers in mind:
Medication Reconciliation:
It's essential to complete the medication reconciliation process before the face-to-face visit. This ensures that any potential medication discrepancies or interactions are identified and addressed promptly, contributing to patient safety and effective care coordination.
Eligible Settings:
TCM services and the associated CPT codes can be initiated and billed under several settings, including:
-
Discharges from acute care hospitals
-
Discharges from inpatient rehabilitation facilities
-
Discharges from long-term care hospitals
-
Discharges from skilled nursing facilities (SNFs), including distinct part units of a hospital
-
Partial hospitalization at a Community Mental Health Center (CMHC)
Medical Decision Making:
Accurately documenting the level of medical decision-making complexity is critical for choosing the correct CPT code. Be sure to include details about the number of diagnoses, treatment options, and the risk of complications involved in the patient's care.
Exclusions:
TCM services cannot be billed concurrently with:
-
Home health care supervision CPT codes
-
Hospice care plan oversight CPT codes This is because these services inherently encompass elements of care coordination and management that overlap with TCM services.
30-Day Discharge Period:
TCM services must be initiated within two business days of discharge and completed within 30 days of the discharge date. It's vital to adhere to this timeframe to ensure eligibility for billing these codes.
What If the Patient Is Readmitted Within 30 Days?
Patient readmissions within the 30-day TCM service period can create billing complexities. Let's clarify how to handle such scenarios:
Scenario 1: Readmission Before Face-to-Face Visit
If the patient is readmitted before the required face-to-face visit is conducted, you cannot bill for either CPT code 99495 or 99496. The face-to-face visit is a mandatory component of both codes, and its absence disqualifies the service from being billed as TCM.
Scenario 2: Readmission After Face-to-Face Visit
If the patient is readmitted after the face-to-face visit has taken place, you can still bill for the appropriate TCM code, provided all other requirements are met. However, the following conditions apply:
CPT 99495 Requirements:
-
The initial face-to-face visit must have occurred within 14 days of the original discharge date.
-
All other non-face-to-face TCM services must have been provided within 30 days of the original discharge date.
CPT 99496 Requirements:
-
The initial face-to-face visit must have occurred within 7 days of the original discharge date.
-
All other non-face-to-face TCM services must have been provided within 30 days of the original discharge date.
Words By Author
In the end, mastering TCM billing with CPT codes 99495 and 99496 comes down to understanding the rules of the game. It's about clear documentation, timely action, and knowing when those codes are applicable (and when they're not). By taking the time to familiarize yourself with the guidelines and best practices we've outlined, you can navigate this billing landscape with confidence.
Remember, your focus should be on providing top-notch care to patients during their transition home – and accurate billing ensures you're fairly compensated for that essential work.
ABOUT AUTHOR

John Wick
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.