For providers, the challenge lies in translating clinical observations into codes that reflect the diagnosis and contributing factors. Are you documenting constipation due to medication use? Is it associated with a specific gastrointestinal condition?
Does your documentation support the severity or chronic nature of the case? These nuances matter not just for coding compliance but also for effective patient management and practice efficiency.
In this guide, we’ll break down the ICD-10 codes that apply to constipation and explore their appropriate use. Whether you’re addressing routine cases or managing complex presentations, this resource will help you code with confidence and precision.
What is the First-Line ICD-10 Code for Constipation?
The primary ICD-10 code for constipation is K59.00 (Constipation, unspecified). This code is used when a patient presents with constipation, but the exact type or underlying cause hasn’t been determined or documented. It serves as a general, first-line option for coding constipation in its most basic form.
Let's explore further classifications in coding for constipation
Slow Transit Constipation ICD 10 Code
When it comes to slow transit constipation, the appropriate ICD-10 code is K59.01. This condition is characterized by a delay in the movement of stool through the colon, leading to symptoms such as infrequent bowel movements and difficulty passing stools despite adequate effort.
Outlet Dysfunction Constipation ICD 10 Code
For constipation caused by outlet dysfunction, the appropriate ICD-10 code is K59.02 The K59.02 code is used when there’s a clear indication that the patient’s constipation stems from issues like pelvic floor dysfunction, rectal prolapse, or impaired coordination of the muscles involved in defecation.
Opioid-Induced Constipation
When it comes to opioid-induced constipation, the appropriate ICD-10 code is K59.03. This code falls under the broader category of drug-induced constipation, which specifically refers to constipation caused by medications. Opioids, in particular, are a well-known cause of constipation due to their effect on the gastrointestinal system, slowing bowel motility.
Coding for Acute vs. Chronic Constipation
For acute constipation, the appropriate ICD-10 code is K59.00 (Constipation, unspecified). This code is used when the constipation is of sudden onset, and the underlying cause has not been clearly defined.
When it comes to chronic constipation, it’s important to categorize it correctly. The most commonly used code for chronic idiopathic constipation, also known as functional constipation, is K59.04. This code applies when the constipation is chronic and no specific underlying medical condition is identified, making it a functional disorder.
ICD 10 Code For Fecal Impaction
The ICD-10 code for fecal impaction is K56.41. This code is used when there is a large, hard mass of stool that cannot be passed naturally, leading to obstruction in the colon or rectum. It is important to document the condition thoroughly to support the correct use of this code, as fecal impaction is often a complication of chronic constipation.
IBS with Constipation ICD 10
For Irritable Bowel Syndrome with Constipation (IBS-C), the ICD-10 code is K58.0. This code is used when a patient is diagnosed with IBS, and constipation is the predominant symptom. It’s important to differentiate IBS-C from other forms of constipation, as the treatment and management approach can vary.
ICD-10 Coding Guidelines for Constipation
When coding for constipation, precise and accurate documentation is essential to ensure correct billing and proper reimbursement. Below are expert coding guidelines to follow when documenting constipation cases:
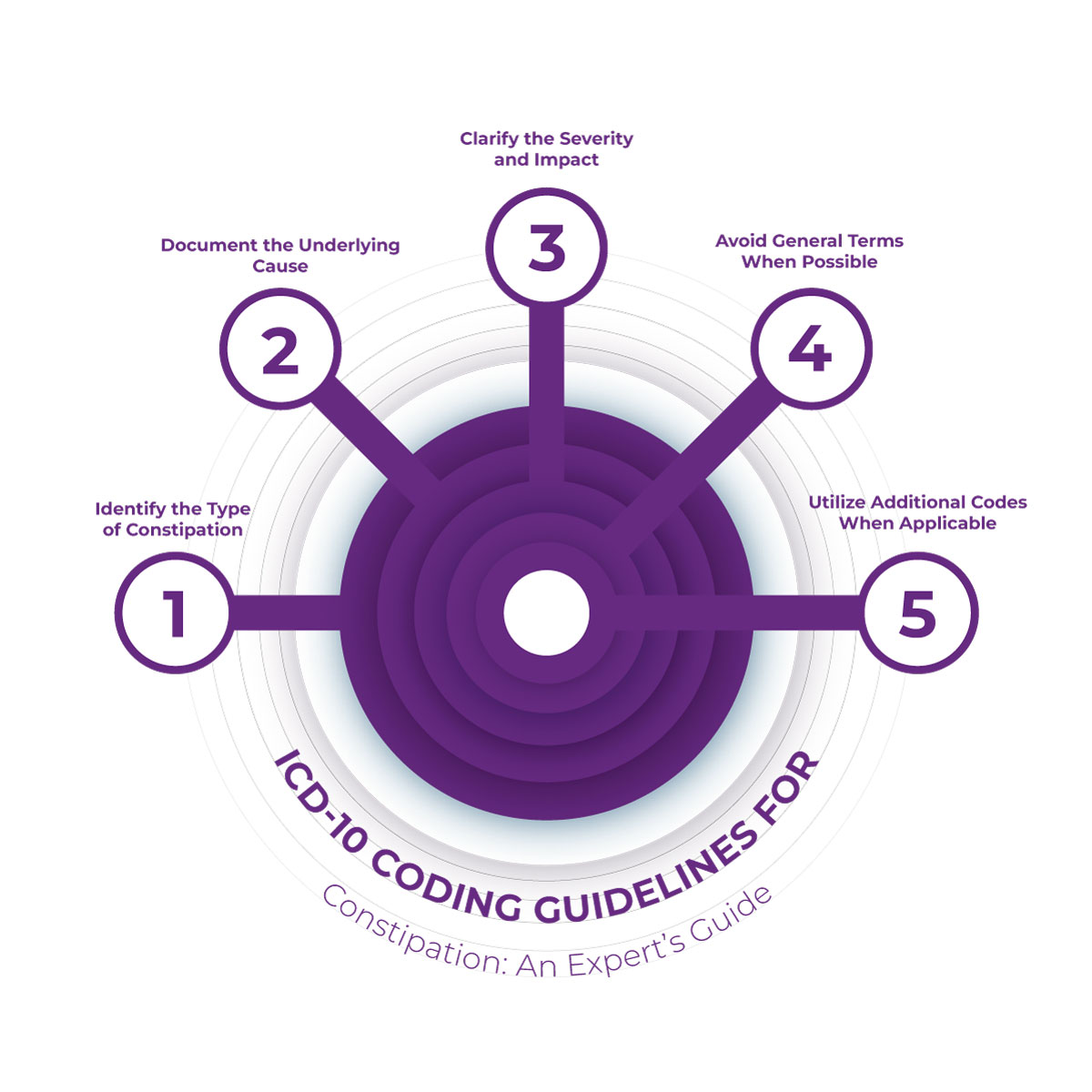
1. Identify the Type of Constipation
-
Acute vs. Chronic: It's crucial to distinguish between acute and chronic constipation. Acute constipation typically has a sudden onset, whereas chronic constipation persists for longer periods and often requires specific documentation of its duration and impact on the patient. Accurate differentiation between these two categories can help in selecting the appropriate code.
-
Functional vs. Secondary: Determine whether the constipation is functional (idiopathic) or due to an underlying condition. Functional constipation does not have a specific cause, while secondary constipation may be due to factors like medication use, gastrointestinal disorders, or systemic diseases.
2. Document the Underlying Cause
-
Medication-Related: If constipation is due to medications, such as opioids or other drug classes known to cause constipation, this should be clearly documented. Identifying the drug as the cause allows for precise coding.
-
Systemic or GI Conditions: If the constipation is related to a gastrointestinal disorder like irritable bowel syndrome (IBS) or is secondary to other medical conditions, it’s essential to document the condition clearly to reflect the cause of the constipation.
3. Clarify the Severity and Impact
-
Duration and Frequency: Chronic constipation should be documented as such, noting how long the symptoms have been present and how frequently they occur. Acute cases should also specify the duration and whether the symptoms are temporary or require immediate intervention.
-
Complications: If the constipation has led to complications, such as fecal impaction or bowel obstruction, it is crucial to document this to ensure proper coding of these conditions alongside the constipation diagnosis.
4. Avoid General Terms When Possible
-
It is important to avoid vague terms like “constipation” without further explanation. Always strive to specify the type (e.g., functional, drug-induced, chronic) and any contributing factors. General codes should be used only when no further specifics are available, but these should be the exception rather than the rule.
5. Utilize Additional Codes When Applicable
-
If constipation is secondary to another condition, such as rectal prolapse or a systemic disorder, make sure to document and apply any additional relevant codes. This can help capture a more comprehensive view of the patient’s condition and prevent under-coding.
ABOUT AUTHOR

Pedro Collins
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.