Mental health is a crucial part of overall health and well-being. Yet, physicians are often reluctant to utilize services for mental health billing due to the complexities and difficulties involved in the process.
To ensure that their patients have access to the necessary care and resources, physicians must become educated about the intricacies of mental health billing.
Mental health billing revolves around accurately coding services, understanding reimbursement regulations, and navigating the complexities of insurance companies. It is also essential to ensure that all procedures are conducted with compliance to avoid potential issues or penalties.
To get started, physicians should evaluate their current billing environment and determine whether they need additional support. So let’s deep down into this article and get an understanding of mental health billing and why physicians need to outsource their mental health billing services.
Understanding Mental Health Billing
Mental health services are an essential aspect of providing comprehensive care to patients who are struggling with mental health issues. Understanding the mental health billing process can help physicians navigate the complexities of insurance coverage, reimbursement, and claims processing.
- The first step in the mental health billing process is determining the patient's insurance coverage including how much patient responsibility for his/her visit. Patients may have insurance plans that cover mental health services, but there may be limitations on the types of services. For example, some insurance plans may only cover short-term counseling or therapy. In contrast, others may cover a broader range of mental health services, such as psychiatric evaluations and medication management.
- Once the patient's insurance coverage has been determined, the next step is determining the appropriate billing codes for the mental health services provided. This involves using diagnostic and procedure codes that accurately reflect the patient's condition and the provided services.
- The next step in the mental health billing process is to submit a claim to the correct insurance company which will be responsible for the mental health services. This involves providing detailed information about the patient, services, and billing codes used. The insurance company will then review the claim and determine the amount reimbursed to the physician.
It's important to note that the mental health billing process can be complex and time-consuming, especially for physicians who are already managing a busy practice. This is why many physicians work with mental health billing service providers specializing in handling insurance claims and reimbursement processes.
Who Can Bill Medicare for Mental Health Services?
For providers, if you are going to bill mental health services like diagnostic and therapeutic treatment or conducting diagnostic exams and other SBIRT services, Medicare has established a list of part B providers eligible to bill them for mental health services.
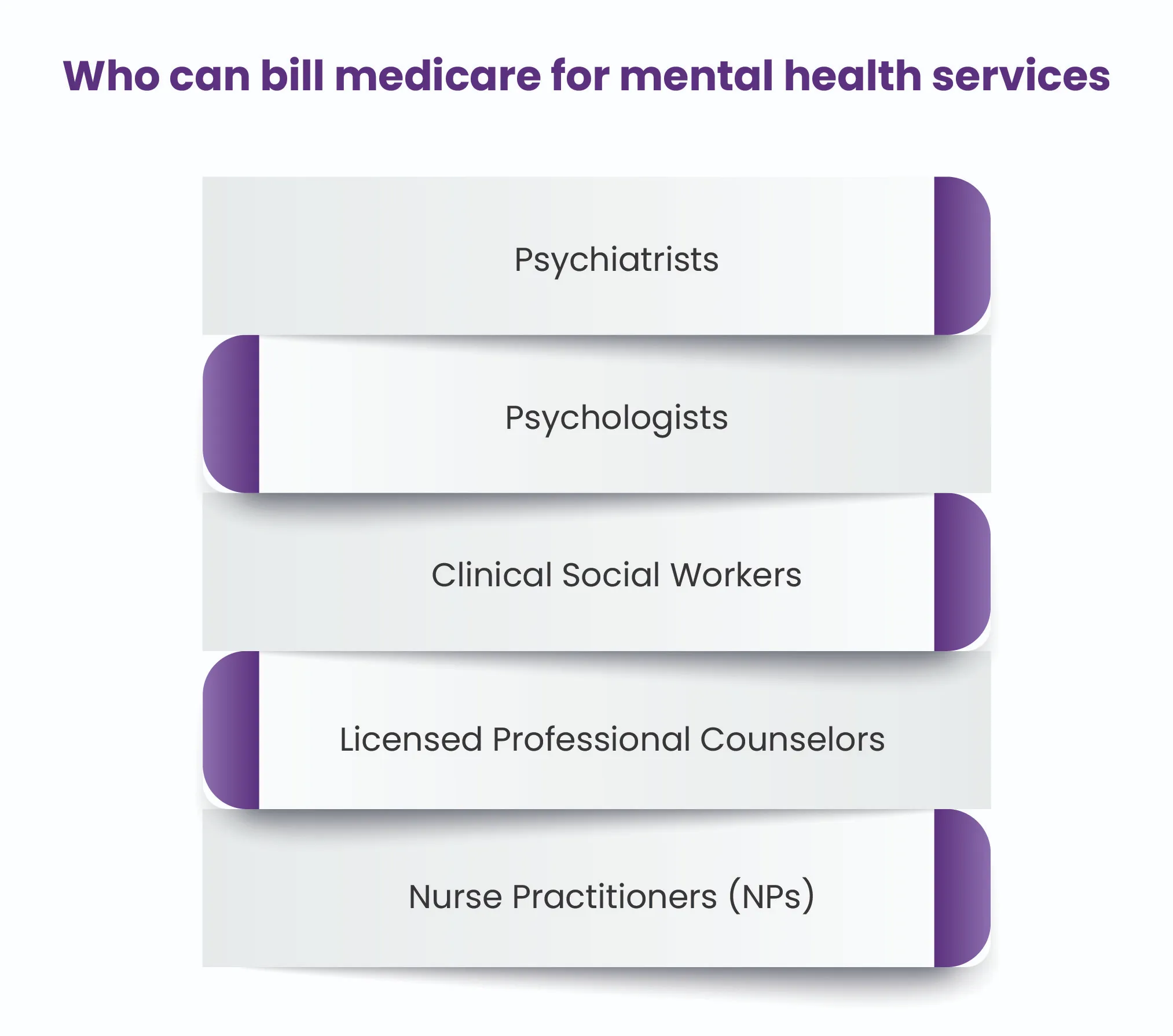
Psychiatrists - Psychiatrists are medical doctors who specialize in the diagnosis and treatment of mental illnesses. They can provide individual psychotherapy and prescribe medication if necessary.
Psychologists - Psychologists are mental health professionals with a doctorate in psychology. They can provide individual and group psychotherapy but cannot prescribe medication.
Clinical Social Workers - Clinical Social Workers are mental health professionals with a master's degree in social work. They can provide individual and group psychotherapy.
Licensed Professional Counselors - Licensed Professional Counselors are mental health professionals who hold a master's degree in counseling. They can provide individual and group psychotherapy.
Nurse Practitioners (NPs) - Nurse Practitioners are advanced practice registered nurses with a master's degree in nursing. They can provide individual psychotherapy, conduct diagnostic exams, and other services.
Most Commonly Used CPT Code in Mental Health Billing
Using proper Current Procedural Terminology (CPT) codes is crucial for accurately billing mental health services provided to patients. Out of the numerous CPT codes available, the following nine codes are the most frequently used for psychiatric and therapeutic services:
- 90791 - This code represents an initial psychiatric evaluation lasting 45-50 minutes.
- 90792 - This code is used for a follow-up psychiatric evaluation, typically shorter in duration than the initial evaluation.
- 90832 - This code is used for a 30-minute psychotherapy session with a patient.
- 90834 - This code represents a 45-minute psychotherapy session with a patient.
- 90837 - This code is used for a 60-minute psychotherapy session with a patient.
- 90846 - This code is used for family psychotherapy with the patient present.
- 90847 - This code is used for family psychotherapy without the patient present.
- 90853 - This code is used for group psychotherapy.
- 90839 - This code represents a psychotherapy session with a physician that includes pharmacologic management, such as adjusting medication doses.
It's important to use the correct CPT code as it indicates the specific mental health service provided and ensures accurate billing.
What complexities do mental health providers face due to inaccurate medical billing?
Medical billing is a complex and challenging process, particularly in mental health. Improper medical billing can lead to a number of difficulties for mental health providers, including:
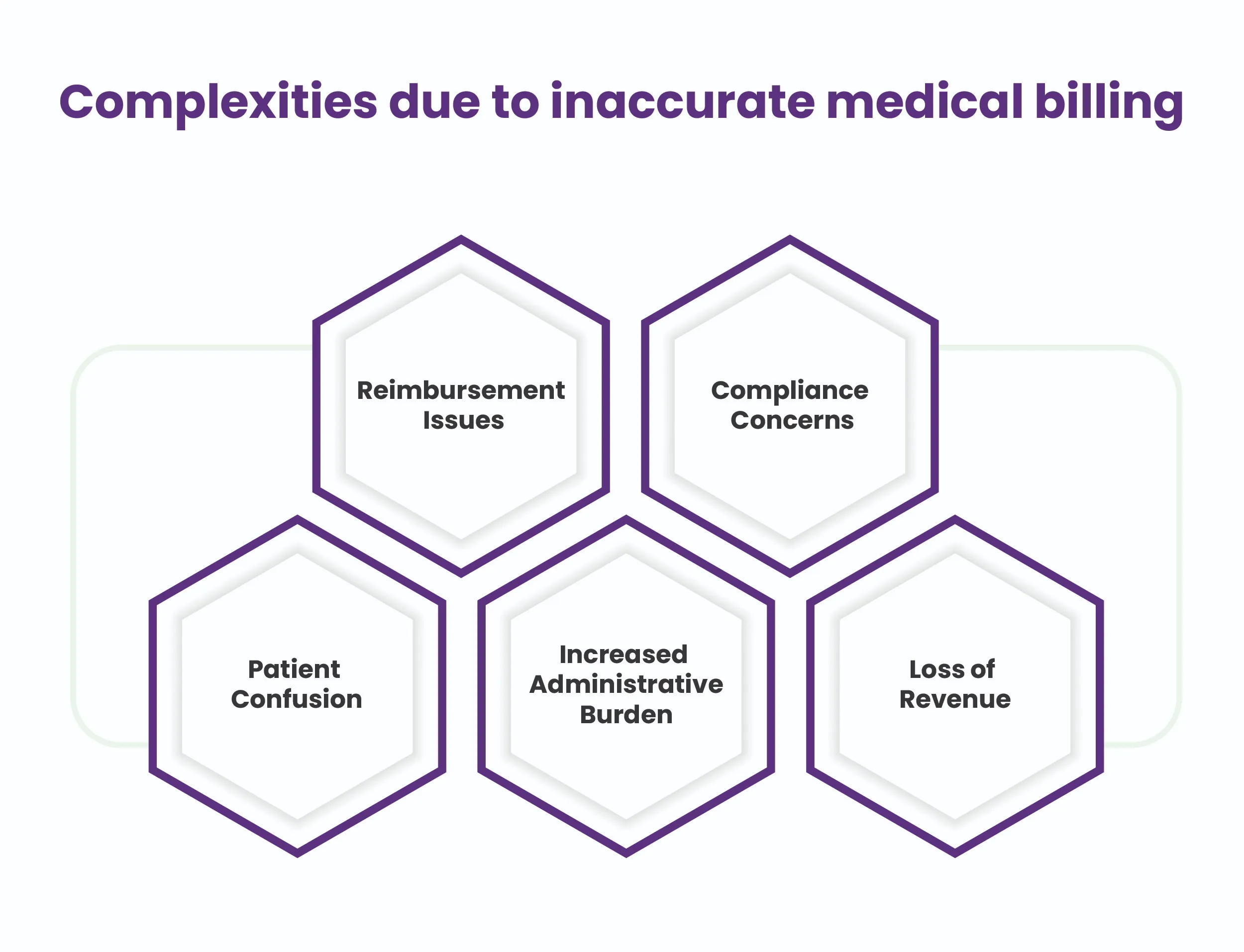
Reimbursement Issues: Improper billing can result in denied claims, delayed payments, and reduced reimbursements. This can put a significant financial burden on mental health providers and can even lead to bankruptcy in some cases.
Compliance Concerns: Mental health billing is subject to strict regulations and laws, such as HIPAA and the Mental Health Parity and Addiction Equity Act. Improper billing can lead to compliance issues that can result in fines and legal trouble.
Patient Confusion: Improper billing can lead to confusion for patients, who may receive unexpected bills or be asked to pay for services they believe were covered by their insurance. This can lead to strained relationships with patients and damage the reputation of the mental health provider.
Increased Administrative Burden: Improper billing can result in increased administrative work for mental health providers, as they may need to resubmit claims or dispute denied claims. This takes time and resources away from providing direct patient care.
Loss of Revenue: Improper billing can result in significant financial losses for mental health providers, as they may need fair compensation for their services. This can impact the sustainability of their practice and limit their ability to invest in the latest technology and equipment.
Advantages of Outsourcing Billing Services for Mental Health Providers
Smooth-sailing mental health billing system is a game-changer for providers! It eases the burden and lets them focus on what matters - delivering top-notch care to patients. Outsourcing billing services can bring several advantages to healthcare providers, which include:
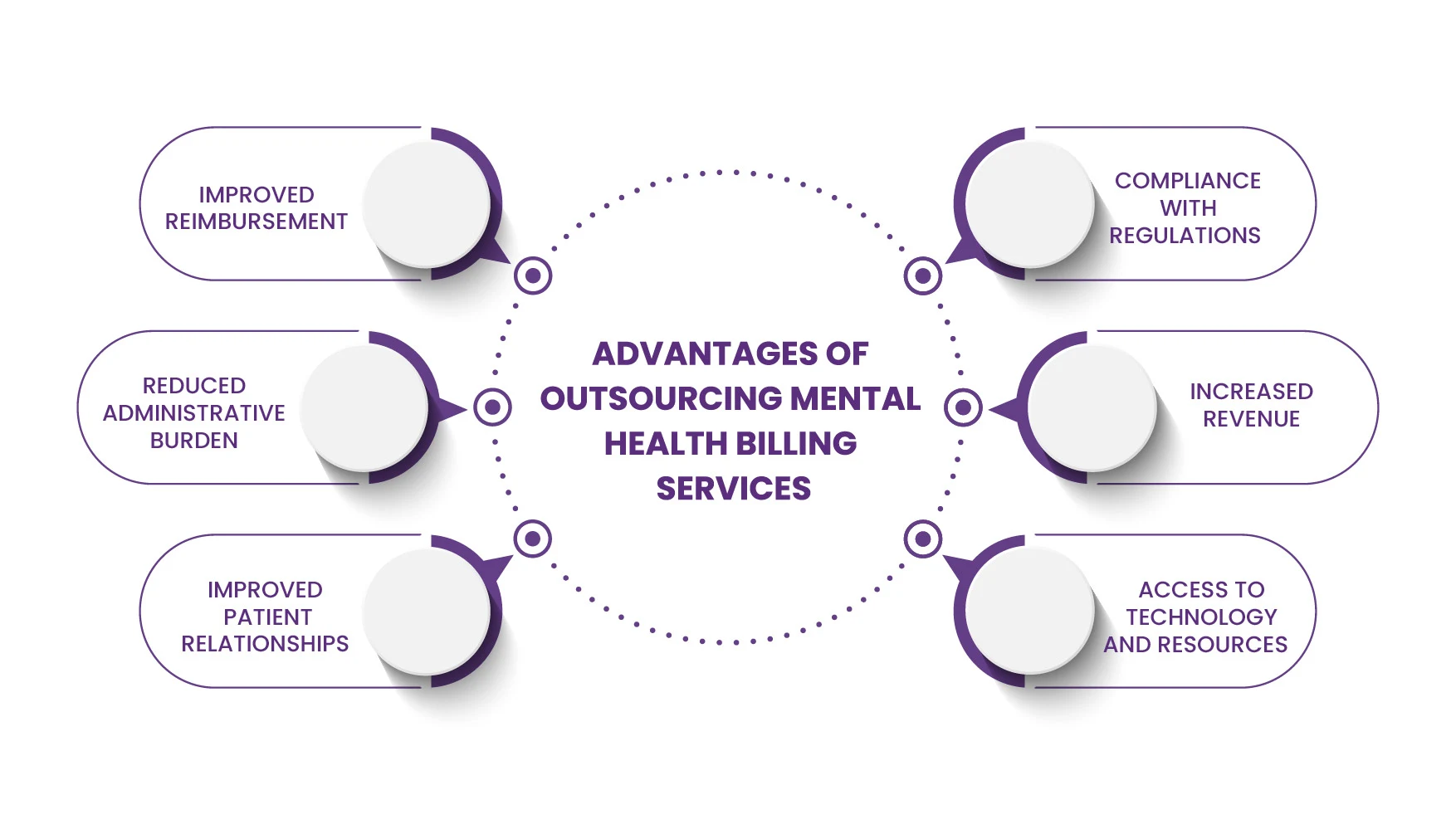
Improved Reimbursement
Working with a specialized mental health billing service provider can increase the accuracy of billing submissions and improve the chances of receiving fair and timely reimbursement for services provided.
Compliance with Regulations
Experts who render these services know the regulations and laws that govern mental health billing, such as HIPAA and the Mental Health Parity and Addiction Equity Act. They can help ensure mental health providers comply with these regulations and avoid legal trouble.
Reduced Administrative Burden
Mental health billing services can handle the administrative tasks associated with billing and claims processing, freeing up mental health providers to focus on providing direct patient care.
Increased Revenue
By improving the accuracy of billing submissions and reducing the number of denied claims, mental health billing services can help increase the revenue of mental health providers.
Improved Patient Relationships
By ensuring that patients receive accurate bills and are not asked to pay for services they believe were covered by their insurance, mental health billing services can help improve patient relationships and maintain a positive reputation for mental health providers.
Access to Technology and Resources
Working with a mental health billing company can provide mental health providers with access to the latest technology and resources, such as electronic health records and financial management tools.
Final Thoughts
Running an efficient mental health billing system is essential for the sustainability of any mental health provider. Outsourcing to a specialized mental health billing service can bring several advantages, such as improved reimbursement, compliance with regulations, reduced administrative burden, increased revenue, and improved patient relationships.
If you're looking for reliable mental health billing services, contact HMS USA LLC today. We'll get you on the path to success with our comprehensive billing services and expertise.
ABOUT AUTHOR

John Bradshaw
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.
