The National Correct Coding Initiative (NCCI) represents one of Medicare's most sophisticated claim review mechanisms, silently evaluating every code pair you submit against a database of over 1.5 million code relationships.
In this comprehensive guide, we will walk you through everything from the fundamental structure of NCCI edits to advanced modifier strategies that can legitimately bypass these restrictions when clinically appropriate.
What Are Medicare NCCI Edits?
The National Correct Coding Initiative (NCCI) was implemented by the Centers for Medicare and Medicaid Services (CMS) in 1996 to promote correct coding methodologies and reduce improper payments for Medicare Part B claims. NCCI edits are essentially rules that define which code pairs can and cannot be reported together for the same patient on the same date of service by the same provider.
These edits serve several key purposes:
-
Preventing unbundling: This occurs when providers report multiple procedure codes when a single comprehensive code should be used instead.
-
Eliminating mutually exclusive procedures: These are procedures that cannot reasonably be performed together based on anatomic, temporal, or gender considerations.
-
Ensuring medical unlikelihood: Some procedures are theoretically possible to perform together but are medically improbable or unnecessary to perform on the same day.
Types of NCCI Edits
There are two primary types of NCCI edits that billing professionals must understand:
1. Procedure-to-Procedure (PTP) Edits
PTP edits involve pairs of CPT/HCPCS codes that shouldn't be reported together unless special circumstances exist. Each PTP edit pair consists of:
-
Column 1/Comprehensive Code: The "preferred" procedure code that is payable
-
Column 2/Component Code: The code that will typically be denied as it's considered part of the comprehensive service
For example, if a surgeon performs a complex abdominal procedure (Column 1), it would typically include the incision and closure (Column 2). Billing both would constitute unbundling.
2. Medically Unlikely Edits (MUEs)
MUEs define the maximum units of service that a provider would report for a single beneficiary on a single date of service in most circumstances. For instance, an MUE might specify that only one appendectomy procedure can be billed per patient per day (which makes anatomical sense).
How CMS Bundling Rules Work
CMS bundling rules, which form the foundation of NCCI edits, follow a logical framework:
-
Comprehensive/component principle: When a comprehensive service is performed, all component procedures integral to that service are considered bundled.
-
Clinical standards: Many edits are based on established clinical practice and anatomical realities.
-
Documentation guidelines: Proper documentation must support any circumstances warranting separate payment.
CMS updates these bundling rules quarterly, making it essential for billing departments to stay current with changes. Updates can include new edit pairs, changes to existing pairs, or removal of obsolete pairs.
Using Modifiers to Bypass NCCI Edits
In certain clinically appropriate situations, providers can bypass NCCI edits by appending specific modifiers. However, modifier use must be supported by documentation showing that the circumstances genuinely warrant separate payment.
Common NCCI-Related Modifiers:
Modifier 59 (Distinct Procedural Service): Perhaps the most widely used NCCI-related modifier, indicating that procedures or services that are not normally reported together were distinct or independent from each other. Because of potential overuse, CMS introduced the X modifiers to provide more specificity.
X Modifiers (Effective January 1, 2015):
-
XE: Separate Encounter
-
XS: Separate Structure
-
XP: Separate Practitioner
-
XU: Unusual Non-Overlapping Service
Other Important Modifiers:
-
Modifier 25: Used with E/M services to indicate a significant, separately identifiable evaluation and management service performed on the same day as a procedure
-
Modifier 51: Multiple procedures performed on the same day
-
Modifier 91: Repeat lab tests performed on the same day
An edit pair's status as "modifier allowed" or "modifier not allowed" determines whether the claim can be bypassed with an appropriate modifier. This status is indicated in the NCCI tables by a value of "0" (not allowed) or "1" (allowed).
NCCI Edit Pairs
NCCI edit pairs form the backbone of the initiative and are organized into two major categories:
1. NCCI PTP Edits for Physicians
These apply to providers billing under Medicare Part B and include edits for:
-
Evaluation and management services
-
Anesthesia services
-
Surgery codes
-
Radiology services
-
Pathology/laboratory services
-
Medicine services
2. NCCI PTP Edits for Outpatient Hospital Services
These apply to facilities billing under Medicare's Outpatient Prospective Payment System (OPPS) and address similar service categories but with edits specific to the facility setting.
How to Avoid NCCI Denials
Prevention is always better than dealing with denials. Here are practical strategies to minimize NCCI-related claim rejections:
-
Implement front-end claim scrubbers: These can flag potential NCCI issues before submission.
-
Regularly download and update NCCI edit tables: CMS publishes quarterly updates that should be incorporated into your billing system.
-
Educate providers and coders: Ensure everyone understands NCCI principles and documentation requirements, especially for modifier use.
-
Review denial patterns: Analyze NCCI-related denials to identify recurring issues in your practice.
-
Document medical necessity: Thorough documentation is crucial, especially when using modifiers to bypass edits.
-
Perform internal audits: Regular auditing can help identify coding patterns that might trigger NCCI edits.
-
Consider the complete clinical picture: Code selection should always reflect the full scope of services provided.
The Proper Use of Modifier 59 and NCCI
Modifier 59 warrants special attention due to its frequent use and potential for misapplication. CMS considers this a "modifier of last resort" that should only be used when no more specific modifier is appropriate.
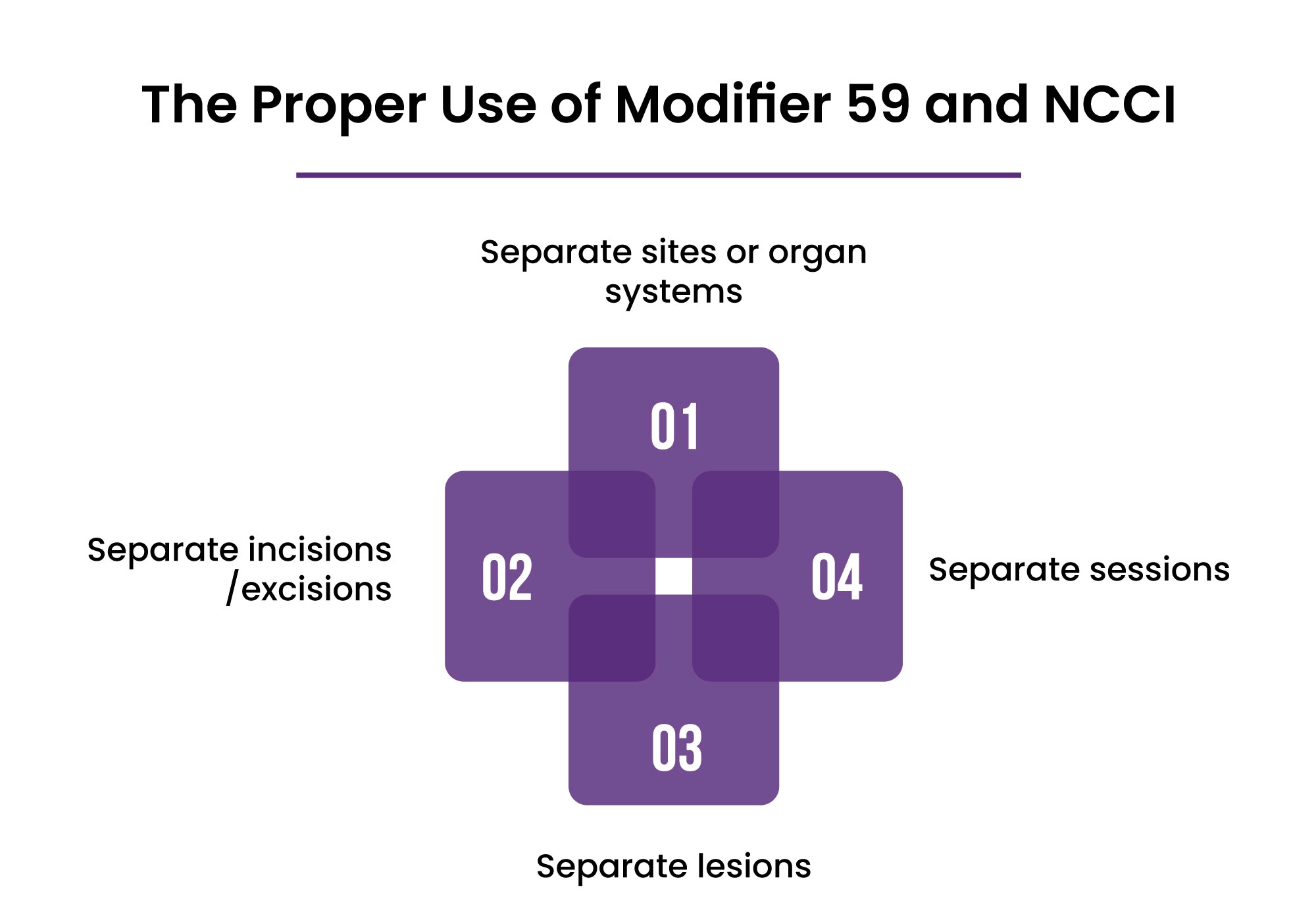
Proper use of Modifier 59 requires:
-
Separate sites or organ systems: The procedures were performed on different anatomical sites or organ systems.
-
Separate incisions/excisions: Different incisions or separate excisions were required.
-
Separate lesions: The procedures addressed separate lesions or separate injuries.
-
Separate sessions: The procedures were performed in separate sessions on the same day.
When documentation supports one of these scenarios, Modifier 59 (or the more specific X modifier) can be appropriate. However, if the NCCI edit pair has a modifier indicator of "0," even appropriate use of a modifier will not bypass the edit.
Words By Author
Understanding Medicare NCCI edits is essential for medical billing professionals who want to maximize reimbursement while maintaining compliance. By understanding the principles behind these edits, using modifiers appropriately, and staying up-to-date with updates, you can handle this complex aspect of medical billing successfully.
Remember that NCCI edits aren't just administrative hurdles—they reflect clinical realities and help ensure that Medicare pays only for medically necessary services provided in accordance with established clinical guidelines. By aligning your coding practices with these principles, you'll not only improve your claims' success rate but also contribute to the integrity of the healthcare system.
ABOUT AUTHOR

Pedro Collins
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.