For Medicare-participating clinics, 2025 brings more than regulatory pressure—it brings a chance to turn reporting into revenue.
As MIPS requirements evolve, the right strategy can help practices not only stay compliant but also unlock higher reimbursement
This guide outlines what your practice needs to know about eligibility, timelines, and score optimization in 2025—along with the key mistakes to avoid and how HMS can help you get ahead.
MIPS Eligibility: Are You In or Out?
Not every provider is required to participate in MIPS, but many assume they're exempt when they're not. For 2025, clinicians must report if they:
-
Bill over $90,000 in Medicare Part B charges
-
See more than 200 Medicare patients
-
Provide 200 or more covered services
Exceptions exist for certain Advanced APM participants, newly enrolled providers, and those below the low-volume threshold.
Group vs. individual participation, segment eligibility, and virtual groups all require verification. Don't rely on assumptions. Use CMS's NPI lookup tool.
To ensure a smooth and penalty-free MIPS submission, clinics should take a proactive, quarter-by-quarter approach. Planning early not only prevents reporting errors but allows time to optimize performance data before submission.
Quarterly Planning Breakdown
✅ Q1: Jan–Mar
-
Confirm MIPS eligibility using NPI/TIN lookup
-
Review prior year performance scores and feedback reports
-
Select six quality measures and ensure at least one is outcome or high-priority
✅ Q2: Apr–Jun
-
Map selected measures to EHR workflows and data fields
-
Train staff on documentation needs for PI and IA categories
-
Begin tracking Improvement Activities (90-day minimum)
✅ Q3: Jul–Sep
-
Audit clinical documentation for numerator/denominator accuracy
-
Monitor preliminary scores and benchmark alignment
-
Adjust workflows and fill any data completeness gaps
✅ Q4: Oct–Dec
-
Finalize PI and IA attestation periods
-
Generate and validate reports across all categories
-
Prepare audit-ready files and submit data before the CMS deadline
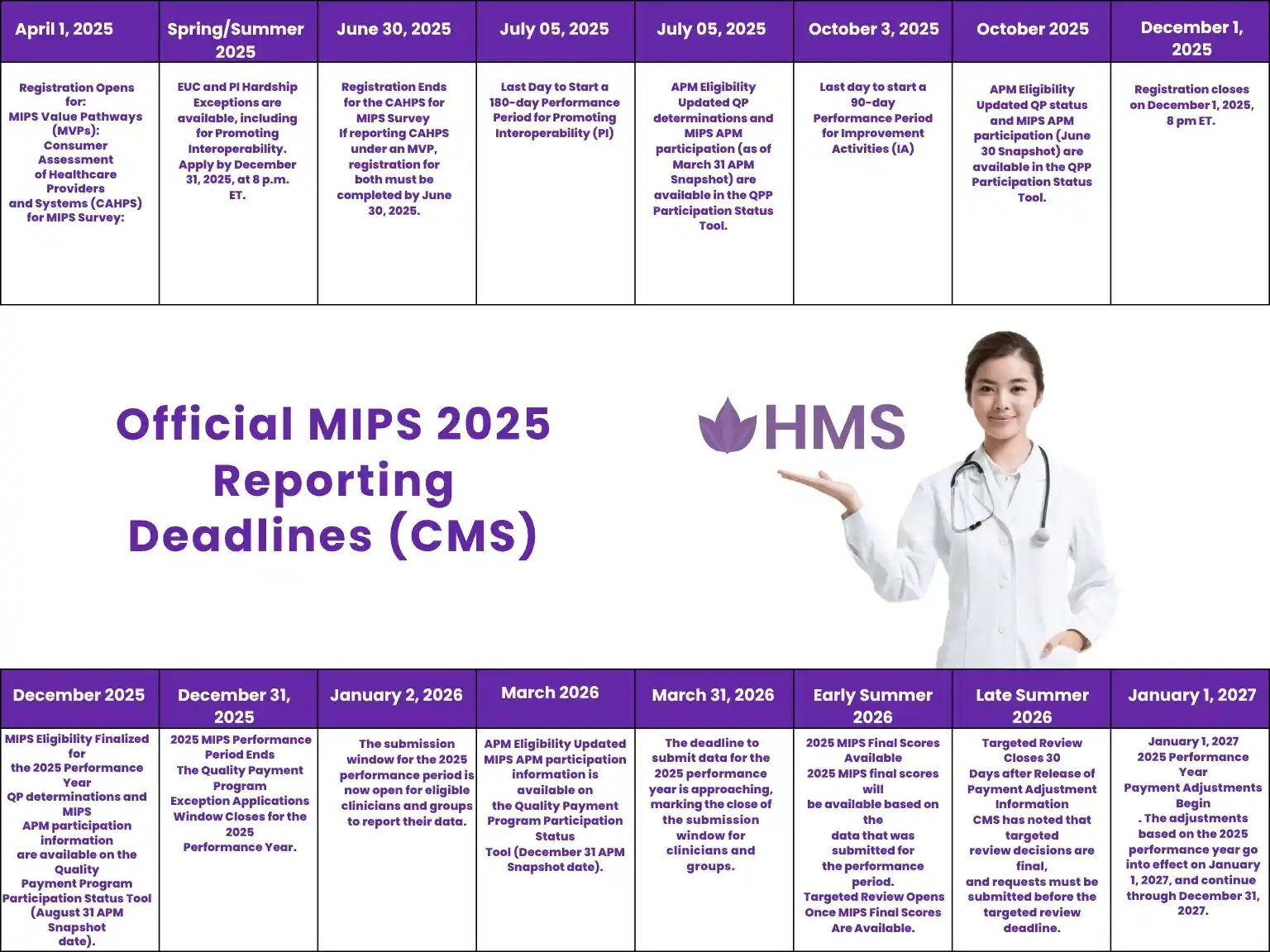
MIPS CMS Deadlines You Can’t Miss
This calendar is based on CMS’s official MIPS 2025 timeline to build trust.
Common Reporting Mistakes That Hurt Your Score
Even compliant providers lose points due to:
-
Topped-out measures: Reporting measures capped at 7 points
-
Incomplete denominator capture: Missing patient data across all payers
-
Low PI performance: EHR issues, staff non-compliance
-
Underreported cost metrics: These are calculated automatically, but documentation still matters
Smart strategy means selecting measures with strong benchmarks and ensuring data completeness across every encounter.
Real-World Example: Avoiding Measure Penalties
If you're a Cardiologist:
Avoid topped-out heart failure or atrial fibrillation measures. Instead, shift to:
#236 (Blood Pressure Control) or #226 (Tobacco Use Screening) — both offer higher decile scoring and broader patient applicability.
If you're a Psychiatrist:
Many clinics overlook measure #371 (Depression Screening) because of workflow gaps. But when tracked properly, it yields strong scoring potential and aligns with behavioral health priorities.
If you're in OB/GYN:
Reporting on chlamydia screening is common, but measure #309 (Weight Screening and Follow-Up) may yield better benchmarks with broader patient coverage.
Choosing the Right Measures – Strategy by Specialty
Not all measures score equally. Strategic selection improves performance without increasing workload. Example:
-
Cardiology: Avoid heart failure measures that are topped-out; focus on blood pressure control or tobacco screening
-
Primary Care: Use flu vaccination and diabetes A1c control for high benchmark potential
-
Psychiatry: Prioritize depression screening with structured follow-up documentation
HMS helps map specialty-specific measures against your documentation habits to maximize scoring potential.
Should You Switch to an MVP Pathway?
MIPS Value Pathways (MVPs) offer streamlined reporting tailored to specific specialties or conditions. Benefits:
-
Reduced measure clutter
-
More relevant benchmarks
-
Easier alignment with clinical focus
In 2025, CMS expanded MVP availability. HMS helps practices evaluate whether to transition to MVP or stick with traditional MIPS based on eligibility, infrastructure, and long-term scoring potential.
How HMS Builds & Executes Your Reporting Strategy
HMS isn't just a billing partner—we act as your strategic MIPS advisor. Our services include:
-
Eligibility & participation verification
-
Measure selection based on benchmark scoring
-
EHR mapping & data completeness audits
-
Decile-based score forecasting
-
Final submission with audit-ready formatting
Our clients routinely outperform national averages and reduce penalty risk by relying on proactive planning and expert oversight.
Final Checklist – Your MIPS Readiness Snapshot
Make sure your clinic is on track across all reporting areas:
-
Eligibility
-
Measure Selection
-
Documentation & EHR Mapping
-
Category Tracking
-
Submission Plan
Need help checking the boxes? HMS offers a free readiness consultation to guide your next steps.
Want to keep this handy?
Download your MIPS Readiness Checklist (PDF) to share with your team or print for internal audits.
Conclusion
MIPS compliance is not just about meeting the minimum—it's about maximizing what you're owed. With the right planning, measure choices, and expert guidance, your clinic can move from "reporting to survive" to "reporting to grow."
Ready to optimize your MIPS strategy? Book a free consultation with HMS
ABOUT AUTHOR

John Wick
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.