Workers' compensation is a system that provides benefits to workers who are injured or become ill due to their job. In the United States, this program is administered by state governments as part of social welfare programs. Under this system, workers do not need to prove that their employer was at fault in order to receive benefits.
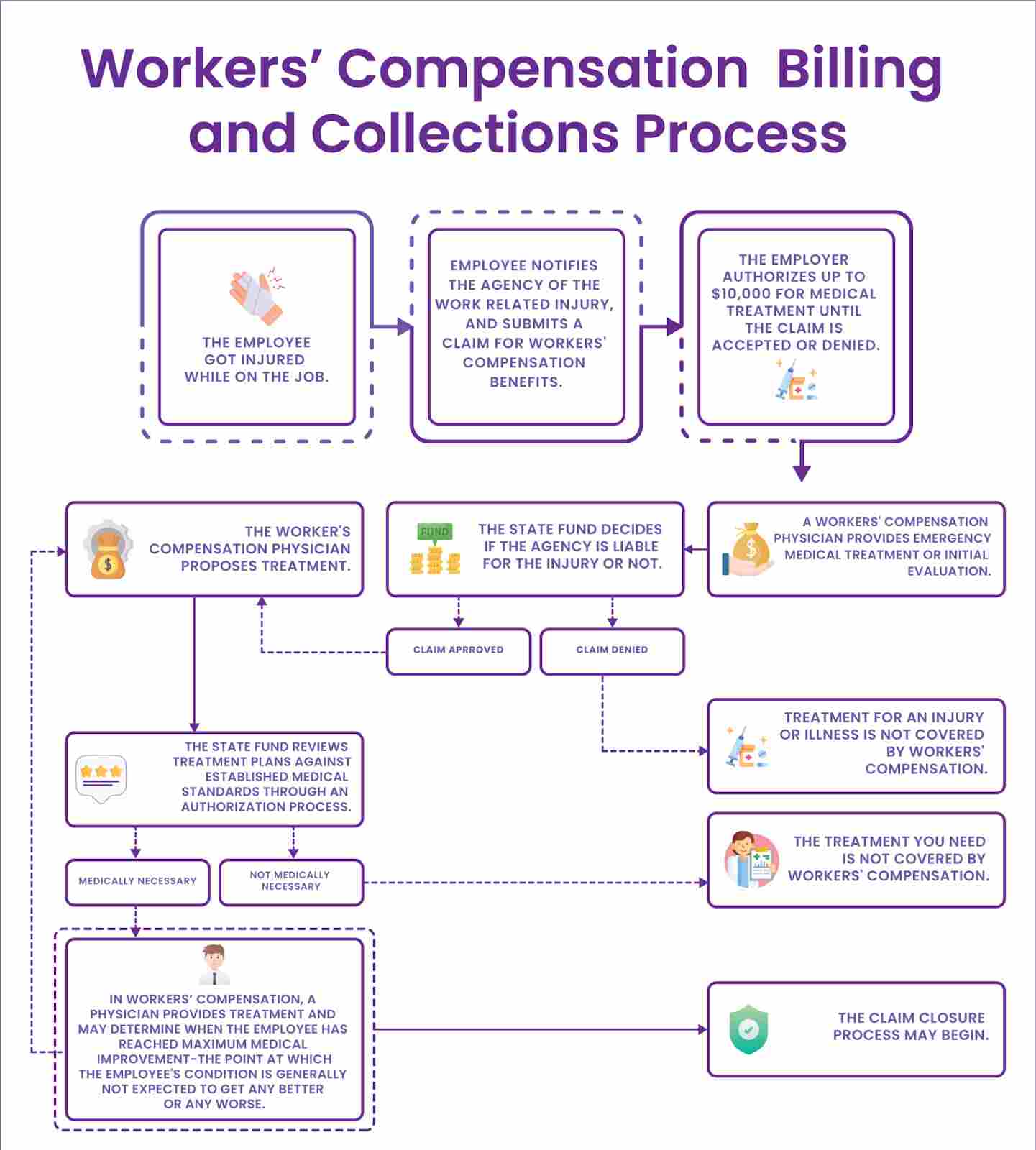
The workers’ compensation billing and collections process starts when the injured worker fills out a claim form and gives it to their employer, and within seven days the employer has to report the injury to their workers' compensation insurance carrier. Once the insurance carrier receives the claim, they will investigate it and decide if they will approve coverage.
Since the workers' compensation billing and collections process can be confusing to understand, HMS USA LLC would like to break it down into two parts:
-
First, we will discuss the workers' compensation billing
-
Second, the collections process.
Furthermore, following the tips outlined in this article, you can streamline your workers' compensation billing and collections process, making it more efficient and effective. Doing so will save you time and money and help to ensure that your business is able to run smoothly.
So, what is workers' compensation billing?
Workers' compensation billing is a process by which the workers' compensation insurance company reimburses the medical provider for the care of an injured worker. This can be done in various ways but usually involves submitting a claim form to the workers' compensation insurance company.
The workers' compensation insurance company will then review the claim and determine whether the claim is compensable. If the workers' compensation insurance company determines that the claim is compensable, they will reimburse the medical provider for the care provided.
It is important to understand that workers' compensation insurances are not obligated to provide coverage for any and all medical treatment recommended by an injured worker's treating physician. Instead, the workers' compensation payor is only required to provide reasonable and necessary medical treatment as determined by the insurance company.
The workers' compensation collections process
Once the care has been provided and the workers' compensation insurance company has decided on compensability, the next step is to begin the collections process. This can be done in a variety of ways but usually involves sending a bill to the workers' compensation insurance company. If the workers' compensation insurance company determines that the bill is payable, they will issue a check to the medical provider for the amount.
A few things can happen if the workers' compensation insurance company determines that the bill is not payable, such as:
-
The first is that the workers' compensation insurance company may deny the bill outright. This means that the workers' compensation insurance company will not pay the bill and the medical provider will have to write it off as a bad debt.
-
The second thing that can happen is that the workers' compensation insurance company may issue a partial payment on the bill. This means that the workers compensation insurance company will pay a portion of the bill, and the medical provider will have to write off the balance as insurance adjustment.
-
The third thing that can happen is that the workers' compensation insurance company may request additional information from the medical provider to determine whether the bill is payable. This additional information may include medical records, treatment notes, and other relevant information.
Once everything has been gathered, the next step is to start the billing process by creating accurate medical coding and submitting the forms to WCB(Workers' Compensation Board).It is important to note that workers' compensation benefits are not automatic, and for an employee to receive workers' compensation benefits, they must first file a claim with their employer.
Forms typical in workers' compensation billing & collections process
Three types of forms were typically used in the workers' compensation billing and collections process:
Form C4 – Used to report the first time you treated a claimant.
Form C4-2 – Used to report continuing services.
Form C4-3 – Used to report permanent impairment.
These forms were revised and replaced with the CMS-1500 on July 1, 2022.The CMS-1500 (08/05) – The new standard claim form that will be used to report all medical services provided on or after July 1, 2022. It is important to note that the workers' compensation insurance company may request additional information from the medical provider to determine whether the bill is payable.
Workers' compensation billing guidelines for providers
These guidelines are for medical providers in billing for services rendered to injured workers under the Workers' Compensation Act. Providers should bill using the CMS-1500 claim form and should include:
Casualty: Providers must state whether they believe the patient became injured or ill while in the scope of their employment or while performing duties related to their job and what happened at work to make them injured or ill.
Work status: The provider must indicate if the patient is currently working, even if it is not at the same job where they were injured or became ill.
Temporary impairment: The provider should indicate the percentage of temporary impairment, if any, when the patient is discharged from care.
-
Providers are expected to use the most current HCPC/CPT coding when documenting services and procedures. This ensures that all services are accurately represented and that patients receive the best possible care.
-
To ensure that the documentation of a code complies with accepted standards, the AMA/CPT guidelines should be consulted.
-
The billing for trauma cases should follow the guidelines by the American College of Surgeons (ACS) and the Pennsylvania Emergency Medical Services (PA EMS).
-
Service Codes from the most recent Bureau Charge-master must be used when submitting claims to the bureau. Providers should familiarize themselves with these codes to submit accurate and timely claims.
-
Insurance companies are not obligated to pay for any treatment until the provider submits a billing on one of the standard forms. This allows the insurance company to properly process the claim and ensure they are paying for a service they agreed to cover.
Workers' compensation billing codes
When an injured worker is seen for an exam related to their disability, the correct medical billing services codes are CPT codes 99455 and 99456. These codes should be reported when "no active management of the problem(s) is conducted during the contact", and when the exam is being used to "obtain baseline information". If the patient does receive additional evaluation and management services during the same visit, then the appropriate E/M or procedure code should be reported in addition to CPT codes 99455 and 99456.
How are workers' comp claims processed and filed?
When it comes to the workers' comp claims processing and filing complexities may arise, so it is vital to have a clear understanding of the requirements before beginning. Here are the basic steps:
-
The injured worker must be seen by a medical provider and evaluated.
-
The medical provider will determine the appropriate treatment plan for the injured worker.
-
The medical provider will then bill the workers' compensation insurance company using the CMS-1500 claim form.
-
The workers' compensation insurance company will then review the claim and determine if it is payable.
-
If the claim is payable, the insurance company will issue payment to the medical provider.
-
If the claim is denied, the medical provider can appeal the decision.
Keep in mind that each workers' compensation insurance company has different requirements and processes for claims, so it is essential to check with the specific insurer before beginning the workers' comp claims process.
How to appeal a workers' compensation denial?
If a workers' compensation claim is denied, the medical provider can appeal the decision. The first step is to request a copy of the denial from the insurance company. The denial should state the specific reason(s) for the denial.Once the medical provider has this information, they can begin to build their case for appeal. The reasons for workers' compensation denial can be various, such as:
-
The service is not covered under the policy.
-
The service is not medically necessary.
-
The patient has not met their maximum medical improvement.
-
The provider did not follow the proper billing and coding guidelines.
-
The provider did not obtain prior authorization for the service.
The flowchart diagram below clearly outlines the workers’ compensation appeals process.
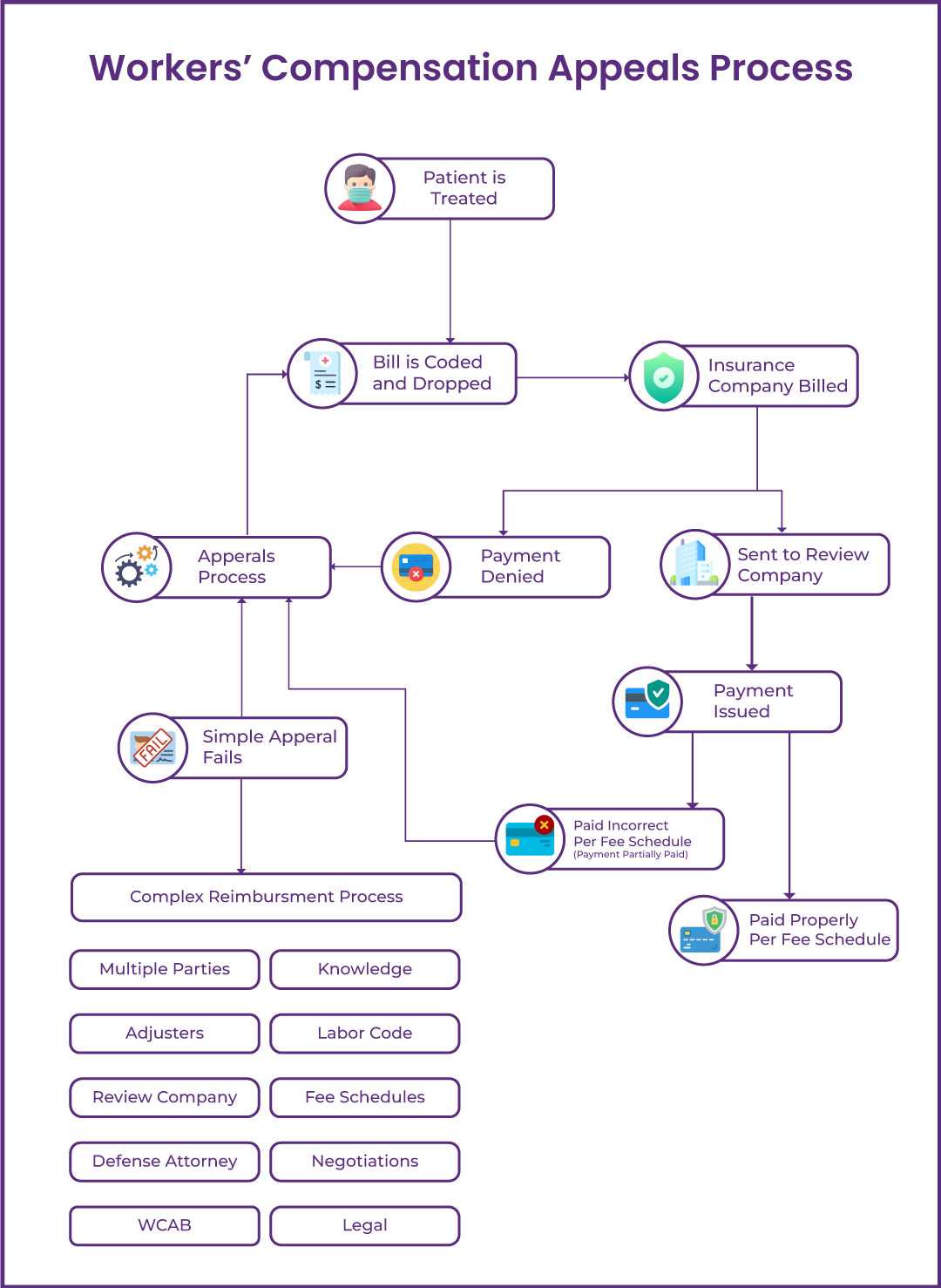
The workers' compensation appeals process can be hard to understand; therefore it is crucial to have a clear understanding of the requirements before beginning. Here are the basic steps:
-
The medical practitioner will first appeal the decision to the insurance company.
-
If the insurance company denies the appeal, the medical practitioner can file a notice of contest with the Workers' Compensation Board.
-
The Board will then review the case and make a determination.
-
If the Board rules in favor of the medical practitioner, the insurance company will be required to pay for the services.
Workers' compensation pros and cons
There are both pros and cons to the workers' compensation system. Some of the pros include:
-
Workers' compensation benefits employees injured on the job, regardless of who is at fault for the accident.
-
It can help employees return to work after an injury.
-
Workers' compensation can help cover the costs of medical care and rehabilitation.
Some of the cons of workers' compensation include:
-
Workers' compensation benefits can be slow to arrive.
-
The benefits may not be enough to cover all of an injured worker's expenses.
-
It may not cover psychological injuries.
Overall, the workers' compensation system provides some benefits to injured employees; however, the drawbacks should be considered before deciding whether or not to file a claim.
Most common challenges faced in workers' compensation billing and collections process?
To streamline the workers' compensation billing and collections process, it is paramount to understand the common challenges faced. By understanding the challenges, you can take steps to avoid or mitigate them. The eight most common challenges are listed below. If you are facing any of these challenges, reach out to a medical billing and coding expert for assistance.
-
After submitting the claim to the worker compensation insurance carrier, you follow-up and get no response. In most cases, you called the insurance carrier and reached voice mails.
-
There is no online portal access for providing Worker compensation claims status, which makes it difficult to track the claim.
-
Lack of proper benefit checking processes for worker compensation claims.
-
Delays in releasing the medical records by the physician's office.
-
Insurance carriers request additional information which is not readily available.
-
Denials from insurance carriers with no clear explanation
-
Payments received from insurance carriers are short payments, and reimbursement rates are low.
The 10 ways to streamline your workers' compensation billing and collections process
Streamlining workers' compensation billing and collections process can be a laborious task, however, there are some key ways to make the process more efficient.
1. Use an integrated workers' compensation billing software:
By using an integrated workers' compensation billing software, you can automate many of the tasks involved in the billing and collections process. This includes submitting claims, checking benefit eligibility, and requesting medical records. The software can also help you keep track of payments and denials.
2. Negotiate with insurance carriers:
If you are not happy with the reimbursement rates offered by an insurance carrier, you can negotiate for a higher rate. This can be done by providing data on comparable reimbursement rates from other carriers.
3. Verify workers' compensation eligibility and benefits:
Before you submit a claim, verifying that the patient is eligible for workers' compensation benefits is essential, and this can help you avoid denials and delays in payment.
4. Use a workers' compensation billing specialist:
A billing specialist can help you with all aspects of the workers' compensation billing and collections process. They can verify eligibility, submit claims, follow up on denials, and appeal denied claims.
5. Understand workers' compensation terminology:
There are a lot of specialized terminologies involved in workers' compensation. It is important to understand terms such as "pre-authorization" and "utilization review" so you can bill correctly.
6. Streamline workers' compensation paperwork:
The paperwork involved in workers' compensation can be overwhelming. To make the process more efficient, create a system for organizing and storing paperwork.
7. Bill workers' compensation electronically:
Electronic billing can help you avoid delays in payment and reduce the amount of paperwork involved in the process.
8. Use workers' compensation clearinghouses:
A clearinghouse can help you file workers compensation claims electronically, verify eligibility, and track payments.
9. Manage workers' compensation denials:
Denials are a common challenge in Workers' Compensation billing. To manage denials, create a system for tracking and appealing denied claims.
10. Follow up on workers' compensation claims:
It is essential to follow up on workers' compensation claims promptly. This includes checking the status of claims, following up on denials, and appealing denied claims.
In case you want to save time and energy the most efficiently, we recommend outsourcing your workers' compensation billing and collections process. We understand entirely how stress-inducing and time-consuming this process can be for a medical provider owing to the complexity of the whole process. HMS USA LLC Medical Billing Company in NY has years of experience in medical billing and coding services, and we can help you optimize medical practice management administrations.
FAQ! Need Help?
Workers' compensation insurance is a type of insurance that provides medical coverage for employees who are injured or become ill while on the job. It can also help cover lost wages if an employee is unable to work due to their injury or illness. Workers' compensation insurance is typically mandatory in most states.
There is no standard way to bill for workers compensation, as each state has different regulations. However, in general, you will need to use the First Report of Injury Form and the CMS-1500 claim form. You can find more information on your state's specific requirements by contacting your state commission.
The workers' compensation insurance carrier will review the claim and determine if it is payable. If the claim is denied, the medical provider can appeal the decision.
The Workmen Compensation Act is a federal law that provides benefits to employees who are injured or become ill while on the job. The act requires employers to provide workers' compensation insurance coverage for their employees.
Each state has different workers’ compensation regulations. You can find more information on your state's specific requirements by contacting your state commission.
The work injury icd 10 code is Z04.2. This code is used to indicate that the patient was seen for an examination and observation following a work accident.
ABOUT AUTHOR

Clark Jorden
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.