A 68-year-old woman collapses in the grocery store checkout line. Witnesses say she "just dropped" without warning. Paramedics arrive to find her alert and oriented, vital signs stable, no evidence of trauma. The emergency department physician documents "syncopal episode, likely vasovagal" and discharges her home with cardiology follow up.
Seems straightforward, right?
But here's where coding gets interesting. That single clinical encounter could be coded at least five different ways, each with dramatically different reimbursement implications. Use the wrong code, and you're leaving thousands of dollars on the table or worse, triggering a compliance audit.
After reviewing over 2,400 syncope cases in the past year and working directly with CDI teams across 47 hospital systems, we've seen this scenario play out repeatedly. The difference between a $6,800 payment and a $13,200 payment often comes down to three words in the physician's documentation.
Let us show you exactly how to code syncope correctly in 2026, avoid the most common pitfalls that trigger denials, and turn vague documentation into compliant, optimized revenue.
Quick Answer: What Is the ICD 10 Code for Syncope?
The primary ICD 10 code for syncope is R55 (Syncope and collapse). This is a billable and specific code used when a patient experiences transient loss of consciousness with spontaneous recovery.
However, and this is critical, R55 should only be used when:
✓ Loss of consciousness is explicitly documented
✓ Recovery was spontaneous (no resuscitation required)
✓ No underlying cause has been identified
✓ The episode is current, not historical
If any of these conditions aren't met, you need a different code. Keep reading because the nuances matter enormously for both compliance and reimbursement.
Understanding R55
Let's start with the basics before we dive into the complex scenarios that trip up even experienced coders.
What R55 Actually Means
R55 falls under the broader category of "Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified" (codes R00 through R99). This placement tells you something important: R55 is a symptom code, not a definitive diagnosis code.
The official ICD 10 CM descriptor reads simply: "Syncope and collapse."
Inclusion terms under R55:
-
Blackout
-
Fainting
-
Vasovagal attack
-
Vasovagal syncope
What this means practically: if your physician documents any of these terms and the patient lost consciousness, R55 is your code.
The Clinical Definition That Determines Code Assignment
Here's what syncope actually is from a clinical standpoint, and why this definition matters for coding:
Syncope = Transient loss of consciousness caused by global cerebral hypoperfusion, characterized by rapid onset, short duration, and spontaneous complete recovery.
Let's break down why each element matters:
"Transient loss of consciousness" means the patient was actually unconscious. Not dizzy. Not lightheaded. Not "almost passed out." Actually unconscious. If your documentation says "near syncope" or "presyncope," you cannot use R55.
"Global cerebral hypoperfusion" means the entire brain temporarily didn't get enough blood flow. This distinguishes syncope from other causes of altered consciousness like seizures (abnormal electrical activity) or strokes (localized vascular problems).
"Rapid onset" typically means seconds to maybe a minute of warning symptoms. This distinguishes syncope from progressive obtundation.
"Short duration" usually means less than 60 seconds of unconsciousness. If someone is unconscious for 10 minutes, start thinking about other diagnoses.
"Spontaneous complete recovery" is huge for coding. If the patient required CPR, cardioversion, or other resuscitation, you're not dealing with simple syncope. You're dealing with cardiac arrest or another acute condition that needs a different primary code.
When R55 Is Billable and When It's Not
Here's a scenario that plays out in medical records departments daily:
Scenario A: "Patient presents to ED with complaint of passing out at home. Wife witnessed patient collapse, was unresponsive for approximately 20 seconds, then woke up spontaneously. Now alert and oriented. Workup negative. Discharge diagnosis: syncope."
Billable? Absolutely. Use R55 as the principal diagnosis.
Scenario B: "Patient reports feeling lightheaded and dizzy this morning. Thought she might pass out but sat down quickly. Did not lose consciousness. Discharge diagnosis: presyncope."
Billable with R55? No. This patient did not experience loss of consciousness. The correct code is R42 (Dizziness and giddiness), not R55.
Scenario C: "Patient with history of syncope two years ago presents for routine physical. No current symptoms."
Billable with R55? No. For historical syncope that is not currently active, use Z86.79 (Personal history of other diseases of the circulatory system).
The distinction between these scenarios has real financial impact.
The Critical Documentation Elements You Must Verify
Before assigning R55, your documentation should clearly support these elements:
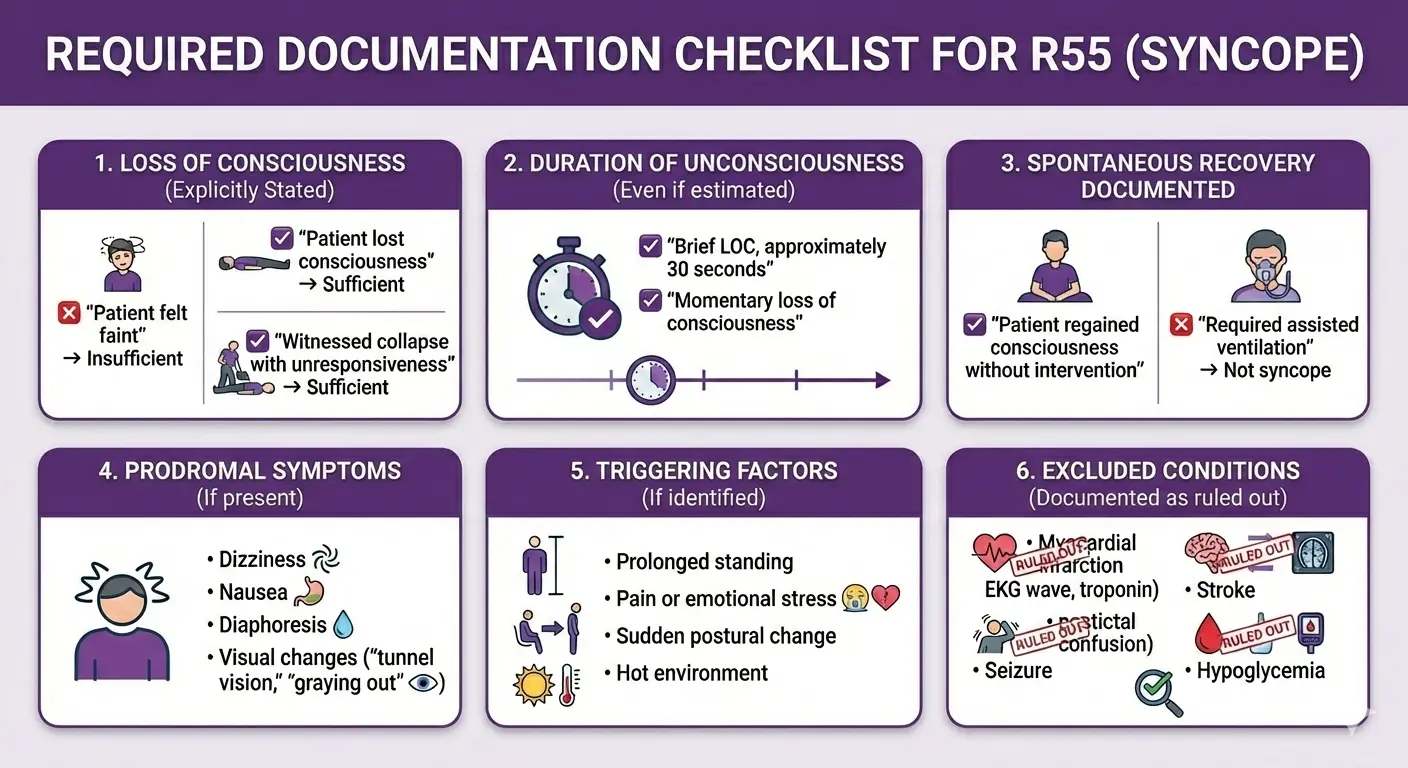
If you're looking at documentation that says only "syncope" with no supporting details, that's your cue for a CDI query. The physician may have all this information in their head, but if it's not in the medical record, it doesn't exist for coding purposes.
Syncope ICD 10 vs Dizziness ICD 10
This is the number one coding error I see in emergency departments and outpatient clinics. Let me make this crystal clear with a comparison table:
|
Clinical Presentation |
Patient Description |
Consciousness Status |
Correct Code |
Common Error |
|
True syncope |
"Everything went black and I woke up on the floor" |
Loss of consciousness occurred |
R55 |
None if documented properly |
|
Near syncope / Presyncope |
"I felt like I was going to pass out but I didn't" |
No loss of consciousness |
R42 |
Incorrectly coding as R55 |
|
Dizziness without syncope |
"The room was spinning" or "I felt off balance" |
Fully conscious throughout |
R42 |
Incorrectly coding as R55 |
|
Syncope with ongoing dizziness |
"I passed out, and I still feel dizzy now" |
LOC occurred, dizziness persists |
R55 (primary) R42 (secondary) |
Only coding one or the other |
|
Lightheadedness |
"I felt woozy and had to sit down" |
Conscious, prevented fall |
R42 |
Incorrectly coding as R55 |
Why This Distinction Matters Beyond Coding Accuracy
It's not just about picking the right code from a book. These conditions have different clinical implications:
Syncope (R55) indicates that cerebral perfusion was actually interrupted. This patient needs a workup to determine why blood flow to the brain was compromised. Cardiac causes, orthostatic hypotension, and neurological conditions are all on the differential.
Dizziness (R42) without loss of consciousness suggests the compensatory mechanisms worked. The patient felt symptoms but never actually lost consciousness. The differential diagnosis is broader and includes vestibular problems, medication side effects, anxiety, and yes, potentially the same cardiac issues as syncope.
From a medical necessity standpoint, syncope justifies a more extensive workup. Insurance companies expect EKG, cardiac monitoring, orthostatic vital signs, and often lab work for R55. For R42 alone, the expected workup is less intensive unless other risk factors are present.
ICD 10 Code for Orthostatic Syncope
Here's where coding gets more sophisticated and frankly, where the money is.
Orthostatic syncope isn't just syncope that happens when someone stands up. It's syncope caused by orthostatic hypotension, a specific physiologic mechanism with its own code.
The Clinical Definition of Orthostatic Hypotension
Orthostatic hypotension is defined as:
-
A drop of ≥20 mmHg in systolic blood pressure, OR
-
A drop of ≥10 mmHg in diastolic blood pressure
-
Within 3 minutes of standing or head-up tilt on a tilt table
This requires actual vital sign documentation. You cannot infer orthostatic hypotension just because someone passed out when they stood up.
How to Code Orthostatic Syncope Correctly
When syncope is documented as due to orthostatic hypotension and you have the vital signs to prove it, here's your coding hierarchy:
Primary diagnosis: I95.1 (Orthostatic hypotension)
Secondary diagnosis: R55 (Syncope and collapse)
Why this order? Because ICD-10-CM guidelines tell us to code the underlying condition (the orthostatic hypotension) before the symptom (the syncope).
Drug-Induced Orthostatic Hypotension
When orthostatic hypotension is documented as caused by medication, you need three codes:
-
I95.2 (Hypotension due to drugs) – primary diagnosis
-
T code(s) for the specific medication(s) with 5th/6th character 5 (adverse effect)
-
R55 (Syncope and collapse) – if loss of consciousness occurred
Common medications causing orthostatic hypotension include:
-
Antihypertensives (ACE inhibitors, ARBs, calcium channel blockers, beta blockers)
-
Diuretics
-
Alpha blockers (often used for BPH)
-
Antidepressants (especially TCAs)
-
Antipsychotics
-
Parkinson's medications (levodopa)
-
Nitrates
Critical coding note: I95.2 specifically states "Hypotension due to drugs" in the excludes note. Do not confuse this with I95.1 (Orthostatic hypotension). If medications are documented as the cause, use I95.2, not I95.1.
ICD 10 Code for History of Syncope: When NOT to Use R55
This is the second most common coding error I encounter, and it's often a compliance risk because it can be seen as upcoding.
The rule is simple: R55 is for current, active syncope. If the patient had syncope in the past and it's not happening now, you cannot use R55.
When to Use Z86.79 Instead of R55
Z86.79 (Personal history of other diseases of the circulatory system) is the appropriate code when:
-
Patient is being seen for a different condition but has a history of syncope that affects clinical decision-making
-
Pre-operative assessment notes prior syncopal episodes
-
Cardiologist sees patient for follow-up after syncope workup was completed and no current symptoms
-
Patient presents for unrelated complaint and mentions "I had a fainting spell a few months ago".
The Compliance Risk of Coding History as Current
Using R55 when you should use Z86.79 is considered upcoding. Here's why:
An active diagnosis of syncope justifies:
-
Emergency department visits
-
Extensive cardiac monitoring
-
Telemetry beds
-
Multiple diagnostic tests
-
Hospital observation status
-
Potential hospital admission
A historical diagnosis of syncope justifies:
-
Notation in the medical record
-
Maybe some additional monitoring during procedures
-
Consideration in medication selection
Vasovagal Syncope: Why It's Still Just R55
We get this question constantly: "Is there a separate code for vasovagal syncope?"
The answer is no, and here's why that's actually good for coders.
Vasovagal syncope is a type of syncope, specifically a reflex syncope where the autonomic nervous system causes sudden vasodilation and/or bradycardia in response to a trigger. Common triggers include:
-
Pain
-
Emotional stress (seeing blood, receiving bad news)
-
Prolonged standing
-
Hot environments
-
Straining (Valsalva maneuver)
In ICD 10 CM, vasovagal syncope is specifically listed as an inclusion term under R55.
This means when your physician documents "vasovagal syncope," you simply code R55. No need to search for a more specific code because the official coding manual tells you R55 is the correct code.
What About Carotid Sinus Syncope?
This is the exception. Carotid sinus syncope has its own code: G90.01 (Carotid sinus syncope).
Use G90.01 only when the physician specifically documents carotid sinus hypersensitivity as the cause, usually after carotid sinus massage testing. This is a very specific neurogenic cause where pressure on the carotid sinus triggers a reflex that causes syncope.
Clinical pearl: In my entire career, I've seen G90.01 coded legitimately maybe 15 times. The vast majority of syncope cases, including those that are clearly reflex/vasovagal in nature, are coded with R55. If you see G90.01 coded frequently in your facility, that's a red flag for potential miscoding that warrants review.
Syncope with Fall and Injury: Adding External Cause Codes
Syncope doesn't happen in a vacuum. When someone loses consciousness, they often fall. When they fall, they may get injured. All of this needs to be captured in your coding.
The Coding Hierarchy for Syncope with Complications
Scenario: 82-year-old woman syncopizes in her living room, falls, and sustains a hip fracture.
Correct coding sequence:
-
S72.001A (Fracture of unspecified part of neck of right femur, initial encounter) – Principal diagnosis because the injury is what's driving the treatment/admission
-
R55 (Syncope and collapse) – Secondary diagnosis, explains why the fall occurred
-
W19.XXXA (Unspecified fall, initial encounter) – External cause code, documents the mechanism
-
Y92.009 (Unspecified place in unspecified non-institutional residence) – Place of occurrence
-
Y93.9 (Activity, unspecified) – Activity code if more specific information isn't available
Why this order? ICD 10 CM guidelines tell us the injury requiring treatment is the principal diagnosis, but you absolutely must code the syncope that caused the fall. If you only code the hip fracture and the fall, you're missing critical information about why the fall occurred, which affects:
-
Fall risk assessment
-
Discharge planning
-
Prevention strategies
-
Future coding if the patient returns
Financial Impact of Complete Coding
Let's look at DRG assignment for the same patient with different coding:
Incomplete coding (injury only):
-
S72.001A (Hip fracture)
-
W19.XXXA (Fall)
DRG: MS-DRG 535-536 (Fractures of hip and pelvis with/without MCC)
Complete coding (injury + cause):
-
S72.001A (Hip fracture) – principal
-
R55 (Syncope) – secondary
-
I95.1 (Orthostatic hypotension) – secondary, if documented
-
W19.XXXA (Fall)
-
Other comorbidities (CHF, COPD, etc.)
DRG: Same MS-DRG 535-536, but now with proper documentation of why the fall occurred, which:
-
Supports medical necessity for the admission
-
Documents fall prevention needs
-
Justifies additional monitoring
-
Captures all conditions affecting the patient
The DRG may not change, but the completeness of the record and the supportability of the admission absolutely does change.
ICD 10 Code for Syncope Unspecified: When R55 Is Your Only Option
Let's be realistic. Sometimes documentation is minimal. The ED is slammed, the physician documents "syncope," and that's all you get despite your best CDI efforts.
In these cases, R55 (Syncope and collapse) is classified as "unspecified" because it doesn't identify an underlying cause. You're documenting the symptom, not the etiology.
This is acceptable coding when:
-
The workup is negative (no cardiac, neurological, or metabolic cause identified)
-
The physician documents syncope but doesn't attribute it to a specific cause
-
Despite appropriate queries, no additional information is available
However, before accepting R55 as unspecified, ask yourself:
-
Was an EKG done? If abnormal, query about the significance
-
Were orthostatic vital signs obtained? If positive, you have I95.1
-
Was any cardiac testing done (echo, stress test, Holter)? If abnormal, query
-
Are there documented comorbidities that could cause syncope? Query for relationship
-
Was the patient on any medications that could contribute? Query about adverse effects
Common Coding Errors and How to Avoid Them
After reviewing thousands of syncope cases, these are the errors I see repeatedly:
Error 1: Coding R55 for Near-Syncope
Wrong: Patient reports "almost passed out" → Coded as R55
Right: Patient reports "almost passed out" with no documented LOC → Code as R42
How to avoid: Always verify loss of consciousness is explicitly documented before using R55
Error 2: Using R55 for Historical Episodes
Wrong: Patient seen for diabetes follow-up, mentions syncopal episode 3 months ago → Coded as R55
Right: Same scenario → Code as Z86.79 (if mentioned at all)
How to avoid: Ask "Is this condition present TODAY during this encounter?" If no, it's historical.
Error 3: Missing the Underlying Cardiac Cause
Wrong: Patient with syncope and documented arrhythmia → Coded as R55 (principal), I48.91 (secondary)
Right: When causation is documented → Code I48.91 (principal), R55 (secondary)
How to avoid: Always query when a potential causative condition is present
Error 4: Failing to Code Orthostatic Hypotension
Wrong: Documentation states "orthostatic hypotension" → Only R55 coded
Right: Documentation states "orthostatic hypotension" → Code I95.1 (principal), R55 (secondary)
How to avoid: Read the entire medical record, not just the problem list
Error 5: Incorrect Sequencing with Injuries
Wrong: Patient syncopizes and breaks wrist → R55 coded as principal diagnosis
Right: Same scenario → S52.501A (wrist fracture) principal, R55 secondary, W19.XXXA (fall) external cause
How to avoid: Remember that injuries requiring treatment are typically the principal diagnosis; code the syncope that caused the fall as secondary
Error 6: Overuse of Unspecified Codes When Specific Codes Exist
Wrong: Patient with documented medication-induced orthostatic hypotension → Coded as R55 only
Right: Same patient → I95.2 (principal) + T code for medication + R55 (secondary)
How to avoid: Always look for documented causes before accepting symptom-only coding
Medicare and Commercial Payer Requirements for Syncope
Different payers have different expectations for syncope workup and documentation. Understanding these requirements prevents denials.
Medicare Guidelines for Syncope
Medical necessity for ED visits: Syncope alone supports Level 4 or Level 5 ED visit (CPT 99284 or 99285) based on:
-
Moderate to high severity problem
-
Moderate to high risk of morbidity without treatment
-
Potential for sudden death if cardiac cause
Expected workup for R55:
-
EKG (required, considered standard of care)
-
Orthostatic vital signs (expected in most cases)
-
Cardiac monitoring (if any cardiac risk factors)
-
Basic labs (CBC, BMP, glucose at minimum)
Observation status criteria: Medicare supports observation for syncope when:
-
Patient has cardiac risk factors
-
Evaluation requires extended monitoring
-
Diagnosis remains unclear after initial workup
-
Patient needs to be observed for recurrence
Two-Midnight Rule: Syncope admissions are generally not expected to meet two-midnight criteria unless:
-
Significant comorbidities present
-
Extensive workup required
-
Hemodynamically unstable
-
High risk features requiring prolonged monitoring
Commercial Payer Considerations
Pre-authorization for advanced testing: Many commercial payers require pre-authorization for:
-
Tilt table testing
-
Electrophysiology studies
-
Implantable loop recorders
-
Cardiac catheterization
Ensure medical necessity is clearly documented with:
-
Recurrent unexplained syncope
-
High-risk features
-
Failed initial workup
-
Suspected serious cardiac cause
Documentation requirements for telemetry: Telemetry monitoring must be justified with documented:
-
Cardiac risk factors
-
Abnormal EKG findings
-
History of arrhythmia
-
Concerning symptoms (chest pain, palpitations)
Simply coding R55 without supporting documentation for high-risk features may result in telemetry denial.
The Bottom Line
After walking through all the nuances, guidelines, and scenarios, here's what you need to remember:
Core Principle: Syncope coding is about clinical accuracy first, revenue optimization second. When you accurately capture the clinical reality, proper reimbursement follows.
The Five Rules of Syncope Coding:
-
Verify loss of consciousness before using R55. If no LOC occurred, use R42 (dizziness), not R55.
-
Code underlying causes as principal diagnosis when documented. Cardiac arrhythmias, orthostatic hypotension, and other specific causes take precedence over the symptom.
-
Distinguish current from historical episodes. R55 is for active syncope; Z86.79 is for history.
-
Document and code all relevant comorbidities. This supports medical necessity, captures HCC risk, and optimizes DRG assignment.
-
Query when documentation is ambiguous. A 30-second query can mean thousands of dollars in appropriate reimbursement.
The Money Shot:
Every syncope case you code is an opportunity to demonstrate the value of accurate clinical documentation. When you code a simple "syncope" case and uncover heart failure, atrial fibrillation, and chronic kidney disease in the process, you're not upcoding. You're accurately representing the clinical complexity of the patient in front of you.
That 68-year-old woman who collapsed in the grocery store? With proper documentation and coding, you ensure she gets appropriate cardiac follow-up, her fall risk is addressed, her medications are reviewed, and your facility is properly reimbursed for the complexity of care provided.
That's not gaming the system. That's excellence in clinical documentation and coding.
Ready to optimize your syncope coding? Start with a focused audit of your last 20 syncope cases. Look for:
-
Cases coded R55 alone where underlying conditions were present
-
Cases where orthostatic vital signs weren't documented
-
Cases where historical syncope was coded as current
-
Cases where potential HCC conditions were missed
The patterns you find will show you exactly where to focus your CDI efforts.
Medical Disclaimer: This content is for educational purposes for healthcare coding professionals. Always refer to the current fiscal year's official ICD-10-CM coding manual, AHA Coding Clinic guidelines, and CMS regulations. Coding should be based on complete physician documentation in the medical record. When documentation is unclear or ambiguous, query the physician for clarification. This article does not constitute medical advice or replace professional coding certification training.
FAQ! Need Help?
Yes, R55 (Syncope and collapse) is a billable and specific ICD 10 CM code valid for the 2026 fiscal year. It can be used as a principal diagnosis or as a secondary diagnosis depending on clinical circumstances.
R55 is the single code for both syncope and collapse. There is no separate code for "collapse" alone. If a patient collapses due to syncope, R55 is the appropriate code.
Syncope (R55) requires documented loss of consciousness. Dizziness (R42) is used when the patient experiences lightheadedness, vertigo, or feeling faint WITHOUT actually losing consciousness. The key distinction is whether LOC occurred.
Yes, but only in specific circumstances. If a patient experienced dizziness that led to syncope AND continues to have dizziness after regaining consciousness, you can code:
-
R55 (principal) for the syncope event
-
R42 (secondary) for the ongoing dizziness
Do not code both if the dizziness was only prodromal (leading up to the syncope) and resolved.
Z86.79 (Personal history of other diseases of the circulatory system) is used for historical syncope that is not currently active. Do NOT use R55 for past episodes.
Each individual episode is coded as R55 for that encounter. If the patient has a pattern of multiple episodes and you're documenting the overall condition, you still use R55 for any acute episode. If discussing historical pattern without a current event, use Z86.79.
Yes. Syncope alone (R55 as principal diagnosis) typically assigns to MS-DRG 312 (Syncope and Collapse) with a relatively low relative weight (~0.68). However, if the underlying cause is identified and documented (cardiac arrhythmia, structural heart disease, etc.), the DRG can change significantly, often with higher reimbursement.
It depends on documentation specificity:
-
If syncope is due to orthostatic hypotension: I95.1 (principal) + R55 (secondary)
-
If due to drug-induced orthostatic hypotension: I95.2 (principal) + T code for drug + R55
-
If orthostatic hypotension is mentioned but syncope is not attributed to it: R55 (principal) + I95.1 (secondary)
When syncope is documented as due to a cardiac condition, code the cardiac condition as principal diagnosis and R55 as secondary. Examples:
-
Syncope due to atrial fibrillation: I48.91 (principal) + R55 (secondary)
-
Syncope due to aortic stenosis: I35.0 (principal) + R55 (secondary)
-
Syncope due to MI: I21.XX (principal) + R55 (secondary)
Use R55. Vasovagal syncope is listed as an inclusion term under R55, so no separate or more specific code is needed.
Only when the physician specifically documents carotid sinus hypersensitivity as the cause, usually after carotid sinus massage testing. This is a rare, specific diagnosis. The vast majority of reflex/vasovagal syncope is coded with R55.
The injury requiring treatment is typically the principal diagnosis, with syncope and external cause codes as secondary:
-
Injury code (e.g., S72.001A for hip fracture) – principal
-
R55 (Syncope and collapse) – secondary
-
W19.XXXA (Unspecified fall) – external cause
-
Place and activity codes as appropriate
No, R55 itself does not map to any HCC category. To capture risk-adjusted revenue, you must document and code underlying conditions that contribute to syncope (heart failure, diabetes, CKD, etc.).
R55 itself is considered "unspecified" because it doesn't identify a specific underlying cause. There is no separate "unspecified" code under R55. If no cause is identified after appropriate workup, R55 is the correct code.
Query when:
-
Documentation is ambiguous about whether LOC occurred
-
A potential underlying cause is documented but relationship to syncope is unclear
-
Orthostatic hypotension is suspected but vital signs aren't documented
-
The timeline is unclear (current vs historical episode)
-
Medication causation is possible but not explicitly stated
Yes, syncope is an acceptable principal diagnosis for observation status when the patient requires extended monitoring to evaluate risk and determine appropriate disposition. Medicare supports this for syncope patients with cardiac risk factors.
ABOUT AUTHOR

Carlos Andrew
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.