According to the 8 minute rule therapy guidelines, a therapist must provide direct, one-on-one therapy for at least 8 minutes to be reimbursed for one unit of a time-based treatment code. This rule also applies to other insurance providers that have specified they follow Medicare billing 8 minute rule therapy standards.
Contrary to this, we have service-based cpt (current procedural terminology) codes that do not have a minimum time requirement associated with them. That means that as long as the service is documented as being provided, it can be billed. These codes are typically used for services that do not require direct, one-on-one time with a patient, such as evaluation or reevaluation codes.
8 minute rule therapy is essential because it helps regulate how many units therapists can bill to Medicare for the outpatient therapy services they provide on a particular service date.
What is 8 Minute Rule?
The 8-minute rule is actually a guideline that healthcare providers can use to bill Medicare for services that take between 8 and 22 minutes. Providers can bill a single unit of services if it lasts more than 8 minutes to 22 minutes. Afterward it would continue in an increment of 15 minutes to bill more units.
Some Restrictions also apply as this rule only applies to certain time-based CPT codes. It's not going to work if you're using the wrong code. And even if you have the right code, you must still meet certain conditions to qualify for the 8-minute rule.
8 minute rule therapy
8-minute rule therapy is a rule that helps therapists determine how many units they should bill to Medicare for the outpatient therapy services they provide on a particular date of service. It might sound simple enough, but things can get tricky when you bill time-based and service-based codes for a single patient.
Let's say, for example, that you have a patient who receives 30 minutes of physical therapy and 4 minutes of service-based initial evaluation on a particular day.
According to the 8-minute rule, you can bill for two units of time-based therapy (30 minutes/15= 2 units) and 1 unit of service-based initial evaluation.
Now let's say that on another day, this same patient receives 18 minutes of therapeutic exercise and 6 minutes of unattended electrical stimulation.
According to the 8-minute rule, you can bill for 1 unit of time-based therapy (18 minutes/15= 1 unit) and 1 unit of untimed service. So, in total, you can bill 2 units.
To minimize the confusion that comes with billing both time-based and service-based codes together, it's imperative to understand how the 8-minute rule therapy works and make sure you're billing correctly.
Timed and untimed Therapy
There are two types of therapy: timed and untimed. Timed therapy is based on the time spent providing the service, while untimed therapy is based on the type of service provided. According to the 8-minute rule, timed therapy must be provided for at least 8 minutes to be billable. This includes all hands-on therapies, such as Manual Therapy and Physical Therapy, while service-based therapy includes all other types of therapies that don't require direct, one-on-one time with the patient.
8 minute rule vs rule of eights
The 8-minute rule is a standard that therapists use to bill Medicare for their outpatient therapy services. This rule states that a therapist must provide direct, one-on-one therapy for at least eight minutes in order to receive reimbursement for one unit of a time-based treatment code.
On the other hand rule of 8s follows the same principles as the 8-minute rule, but it is calculated per service. So, if a therapist provides three different services to a patient, they would need to spend at least eight minutes on each service in order for it to be billable. Primarily, it is a more general standard that applies to all insurances that follow Medicare billing guidelines.
When billing for services, therapists must be aware of the difference between these two standards in order to submit claims accurately, otherwise, they may not be reimbursed for their services.
How to calculate a billable unit?
The 8 minute rule is used to determine how many therapy units should be billed to Medicare for the services provided. To calculate a billable unit, therapists must take the total number of minutes spent providing direct, one-on-one therapy and divide it by fifteen.
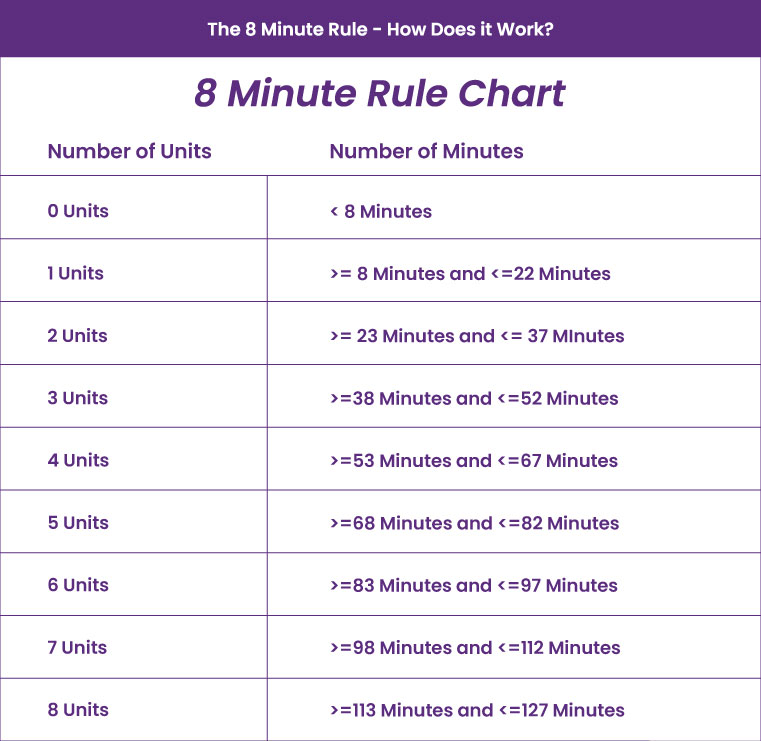
The 8 minute rule chart below outlines the maximum number of units that can be billed according to a given time total.
For example, if a therapist spends thirty minutes providing direct, one-on-one therapy, they would divide thirty by fifteen to calculate that two billable units were provided.
However, if the therapist only spends seven minutes providing direct, one-on-one therapy, they would not bill for a unit of therapy as they have not met the minimum requirement of eight minutes.
Mixed Remainders
When you divide the total timed minutes by 15, you often get a remainder that includes minutes from more than one service. You should only include that remainder in the calculation if it meets the 8-minute rule for one of the services.
For example, let’s say you provided two different services during a 60-minute session and stopped the timer between each service:
Service 1: 15 minutes
Service 2: 3 minutes
Service 3: 5 minutes
You would calculate the number of billables by adding together the time for each service:
15 minutes of ‘Service 1’ + 3 minutes of ‘Service 2’ +5 minutes of ‘Service 3’ = 23 minutes
Then you would divide the total number of minutes (23) by 15 to calculate the number of billable units:
23 minutes ÷ 15 minutes per unit = 1.5 billable units
Here we can bill for a whole 1 unit for ‘Service 1,’ but we are left with a mixed remainder of 8 minutes from 3 minutes of ‘Service 2’ and 5 minutes of ‘Service 3’.
8 minutes is a complete billable unit which means the therapist will bill for 2 units of service. Point to be noted that in the case of mixed remainders, the unit is billed against the service with the biggest time total.
Timed and untimed CPT Codes
In medical coding, there are two types of CPT codes: time-based and service-based. Time-based codes are based on the amount of time spent providing the service, while service-based codes are based on the type of service provided.
Time-based codes are typically used for services that involve continuous hands-on treatment, such as physical therapy. Examples of time-based CPT codes in physical therapy are CPT code 97110 (Therapeutic Exercise), CPT code 97112 (Neuromuscular Re-education ), CPT code 97113 (Aquatic Therapy), etc.
Service-based CPT codes are typically used for services that do not involve continuous hands-on treatment, such as evaluations. Examples of service-based CPT codes in physical therapy are CPT code 97161, CPT code 97162, CPT code 97163, etc.
How to perform PT billing?
The process of billing for physical therapy services can be confusing, especially if you are new to medical billing. In order to bill for physical therapy services, you will need to know the correct codes to use and how to submit them to insurance companies.
To start, you will need to gather the following information:
- The patient's medical records
- The physical therapy codes that correspond to the services you provided
- The patient's insurance information
Once you have gathered all of the necessary information, you will need to submit a claim to the patient's insurance company. The claim should include the physical therapy codes corresponding to the services you provided.
It is important to note that not all insurance companies will cover 8-minute rule physical therapy billing services. If the patient's insurance company does not cover physical therapy, you may still be able to bill the patient directly for the services.
PT billing examples
Let's discuss some great examples for PT billing according to the 8-minute rule:
Suppose a physical therapist gives a patient 3 services during a 60-minute session and stops the timer between each service:
Service 1: 10 minutes
Service 2: 4 minutes
Service 3: 4 minutes
You would calculate the number of billable units by adding together the time for each service:
10 minutes of 'Service 1' + 4 minutes of 'Service 2' +4 minutes of 'Service 3' = 18 minutes
Then you would divide the total number of minutes (18) by 15 to calculate the number of billable units:
You would calculate the number of billable units by adding together time for each service: 10 minutes for Service 1 + 4 minutes for Service 2 + 4 minutes of service 3 = 18 minutes.
Then you would divide the total number of minutes (18) by 15 to calculate the number of billable units:18 minutes ÷ 15 minutes per unit = 1.2 billable units. In this case, you would round up to 1 unit and bill for 1 unit of service.
Let's take another example:
Suppose a physical therapist provides 2 services during a 45 minute session and stops the timer between each service:
Service 1: 30 minutes
Service 2: 15 minutes
You would calculate the number of billables by adding together time for each service:30 minutes for Service 1 + 15 minutes for Service 2 = 45 minutes. Then you would divide the total number of minutes (45) by 15 to calculate the number of billable units:45 minutes ÷ 15 minutes per unit = 3 billable units.
How to avoid problems with physical therapy 8-minute rule billing?
There are a few things that you can do to avoid problems when billing for physical therapy services:
- Make sure you understand the medical billing process before starting billing for services.
- Ensure you understand the 8-minute rule and how it applies to physical therapy services.
- Be sure to keep accurate records of all your physical therapy services.
If you follow these tips, you should be able to avoid any problems when billing for physical therapy services.
Documentation required for Therapy
We understand that documentation can be a huge hassle. After a long day of working with patients and receiving positive feedback about their functional progress, the last thing therapists want to do is sit down and work through the documentation that they couldn’t finish at the point of care. However, this is a very important part of the therapy process. Proper documentation protects the therapist in case of any audit risks that might arise and it also allows for better communication between therapists and other members of the healthcare team.
Some of the required documentation for therapy includes:
- A demographic sheet that has the patient’s name, address, phone number, date of birth, and social security number
- A chief complaint that briefly describes the reason why the patient is seeking therapy services
- An assessment that contains information about the patient’s current level of functioning and what their goals are for therapy
- A plan of care that outlines the therapist’s goals for the patient and what type of interventions will be used to help the patient reach those goals
- Progress notes that document the patient’s progress in therapy, details of all the therapies that were provided, and any changes to the plan of care
- A discharge summary that is completed when the patient is no longer receiving therapy services
Documentation can be time-consuming, but it is an important part of the therapy process. By taking the time to document properly, therapists can protect themselves from any legal issues that might arise and ensure that other healthcare team members are aware of the patient’s progress.
Audit risk with 8-minute rule therapy
Audits are now standard in many industries, and you should be prepared for them no matter your field. Professional billing experts say that the odds are, at some point in your career, you will experience an audit in one form or another. Being proactive and understanding the process can help mitigate any issues that may arise.
Regarding therapy, one of the most common audit triggers is the 8-minute rule. This rule states that the service cannot be considered a billable visit if a patient is seen for less than 8 minutes. So, to avoid audit risks your documentation needs to be thorough enough to prove that the time spent with the patient was adequate.
If you are audited, be sure to cooperate fully and provide any documentation that is requested. If you are able to prove that the services were rendered appropriately, you should not have any problems.
Where does the 8-minute rule apply?
The 8-minute rule applies to all Medicare providers, regardless of whether they are in private practice or working for a hospital or other healthcare facility. This rule is designed to ensure that patients receive the care that they need, and it also protects providers from being overbilled for services that they did not render.
Conclusion
The 8-minute rule is important for both patients and therapists alike. It ensures that patients receive the necessary amount of therapy while also preventing overbilling by therapists. While the rule can be complex, understanding it is crucial for providing quality care.
If you have any further questions about the 8-minute rule therapy, Contact us today@ (212) 363-0114 or you can mail us out at Info@hcmsus.com.
FAQ! Need Help?
The 8-minute rule only applies to Medicare insurance. For other insurances, therapists can bill for according to the rule of eights which states that therapists can bill for 8 minutes of therapy time for each unit of a service-based code.
There are a few exceptions to the 8-minute rule, such as when a patient is discharged from therapy before the end of the session. In these cases, the therapist can still bill for the entire session as long as they document the reasons for the early discharge in the patient's medical record.
The 8-minute rule is not just for Medicare patients. Private insurance companies also use it to determine how many units of a time-based code can be billed on a given day. However, the number of minutes required to make up one unit may vary depending on the insurance company.
The 8-minute rule is a guideline that occupational therapists must follow in order to bill for time-based codes. This means that an occupational therapist must provide at least 8 minutes of direct, one-on-one therapy in order to bill for one unit of a time-based treatment code.
The main difference between medicare and non-medicare insurance is that medicare is a government-sponsored health insurance program for people aged 65 and over, while non-medicare insurance is a private health insurance program. While both programs provide coverage for medical expenses, there are some key differences between them, including the types of coverage they provide, the eligibility requirements, and the costs.
ABOUT AUTHOR

Tammy Carl
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.
