Low Utilization Payment Adjustment (LUPA) has long been a critical element in home health care billing, but its importance skyrocketed during the COVID-19 pandemic. As agencies faced unprecedented challenges—from patients declining visits to staff shortages—LUPA rates climbed from a steady 10% to an alarming 25%.
For many, this exposed the fragile balance between delivering quality care and meeting financial thresholds. LUPA isn’t just a billing adjustment; it reflects how well an agency can adapt to changing circumstances while ensuring sustainable operations. In this blog, we’ll explore what LUPA is, why it matters, and how agencies can avoid the pitfalls of “LUPA land” in both normal and extraordinary times.
What is LUPA?
LUPA stands for Low Utilization Payment Adjustment, a financial adjustment in the Medicare Home Health Prospective Payment System (HH PPS). It occurs when a home health agency provides fewer visits than the minimum threshold required for a specific patient’s billing period. When this happens, instead of receiving a full episodic payment, the agency is reimbursed at a significantly reduced rate, calculated on a per-visit basis.
What is LUPA Threshold Under PDGM Home Health Billing?
Under the Patient-Driven Groupings Model (PDGM) in home health billing, the LUPA threshold refers to the minimum number of visits required within a 30-day payment period to avoid a Low Utilization Payment Adjustment (LUPA). If the number of visits falls below this threshold, the agency receives a reduced reimbursement calculated on a per-visit basis rather than the full episodic payment.
PDGM’s Sliding Scale LUPA Thresholds
In the past, avoiding a LUPA was straightforward: agencies needed to complete more than 5 visits within a 60-day episode to qualify for full episodic reimbursement.With the advent of PDGM, the rules around LUPA thresholds have transformed dramatically, leaving some agencies struggling to adapt. Instead of a fixed visit threshold, the Centers for Medicare & Medicaid Services (CMS) implemented a sliding scale model for LUPA thresholds. The number of visits now required to avoid a LUPA ranges between 2 and 6 visits for each 30-day episode, depending on various patient-specific factors.
What Influences the New LUPA Thresholds?
The new LUPA thresholds are no longer one-size-fits-all. They are determined by:
-
Diagnosis Grouping: The primary reason for home health care, categorized into one of 12 clinical groupings.
-
OASIS Data: Responses to key questions, particularly those in the M1800 section related to functional abilities and limitations.
-
Coding and Comorbidities: Accurate coding of diagnoses and identification of secondary conditions affecting patient care.
Why Avoiding LUPA Is Crucial for Home Health Agencies
Avoiding a Low Utilization Payment Adjustment (LUPA) is critical for home health agencies because it directly impacts both financial stability and the quality of care delivered to patients. Under the Patient-Driven Groupings Model (PDGM), agencies face reduced reimbursement when they fail to meet the required number of visits within a 30-day billing period, which can have far-reaching implications.
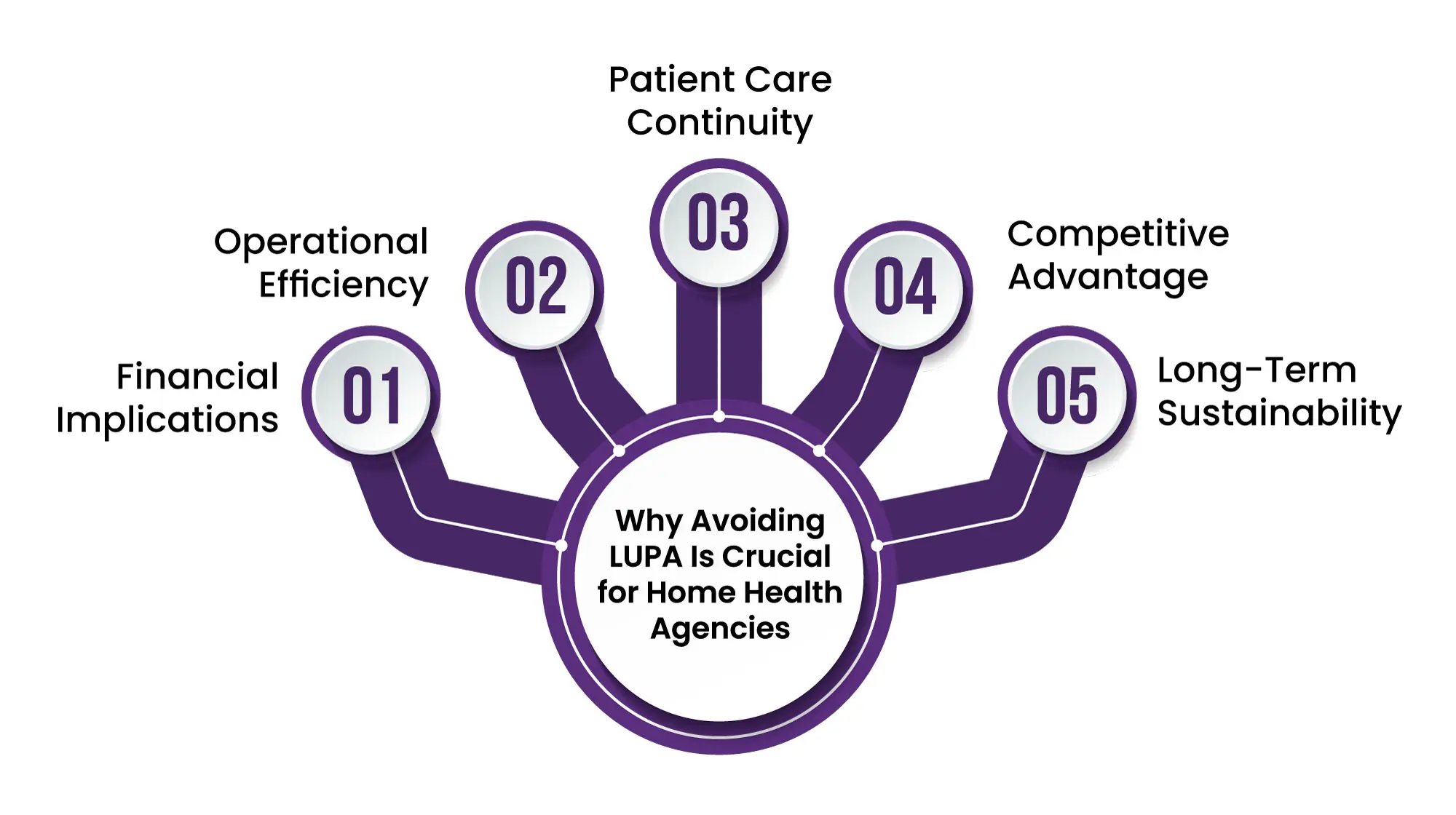
Here’s why avoiding LUPA is essential:
1. Financial Implications
-
Reduced Reimbursement: When a LUPA is triggered, agencies are reimbursed on a per-visit basis, rather than receiving the full episodic payment. This often results in payments that fail to cover the cost of care.
-
Revenue Loss: For agencies operating on tight margins, repeated LUPA occurrences can lead to significant revenue shortfalls, undermining their ability to sustain operations and invest in patient care.
2. Operational Efficiency
-
Care Planning Challenges: Falling below the LUPA threshold indicates inefficiencies in scheduling and resource allocation. Properly planned visits are essential to meet both care goals and billing requirements.
-
Strained Resources: Agencies that frequently encounter LUPAs may experience disruptions in their ability to allocate staff effectively, potentially leading to caregiver burnout and patient dissatisfaction.
3. Patient Care Continuity
-
Reduced Service Delivery: A LUPA may signal fewer patient interactions, which could compromise care quality, delay recovery, or miss opportunities for early intervention in deteriorating conditions.
-
Perceived Value of Care: Meeting visit thresholds ensures patients receive consistent, high-quality care that aligns with their treatment goals, enhancing satisfaction and trust.
4. Competitive Advantage
-
Reputation Management: Agencies that consistently avoid LUPA demonstrate superior care planning and operational excellence, building a stronger reputation in the market.
-
Attracting Referrals: Physicians and hospitals are more likely to refer patients to agencies with a proven track record of efficient and effective care delivery.
5. Long-Term Sustainability
-
Alignment with PDGM Goals: The PDGM model emphasizes value-based care. Avoiding LUPA reflects an agency’s ability to align with these goals, improving their standing with payers and ensuring continued participation in the Medicare program.
-
Risk Mitigation: Proactively managing visits to avoid LUPA reduces financial risk and positions the agency for long-term growth and success.
Proven Strategies to Avoid LUPA in Home Health Care
Avoiding Low Utilization Payment Adjustment (LUPA) requires proactive planning, efficient care delivery, and accurate documentation. By implementing the right strategies, home health agencies can optimize reimbursement, enhance patient care, and improve operational efficiency under the Patient-Driven Groupings Model (PDGM). Here are key strategies to help your agency stay out of "LUPA land”
- Perfect the OASIS Assessment:
Ensure that OASIS data, particularly functional scores (M1800 section), is accurate to determine appropriate thresholds. - Precision in Diagnosis Coding:
Properly code primary and secondary diagnoses to place patients in the correct clinical grouping, optimizing thresholds. - Early OASIS Completion:
Submit OASIS assessments promptly to avoid delays that create blind spots in visit planning. - Strategize Visit Scheduling:
Design a care plan that ensures visits meet the LUPA threshold within each 30-day billing period. - Front-Load Visits:
Schedule a higher number of visits early in the 30-day period to account for unexpected disruptions. - Enhance Low-Visit Cases:
For patients with minimal needs, add supplemental services such as: - Home health aide support.
Routine monitoring of vitals or therapy sessions. - Use Tracking Tools:
Implement software to monitor visit counts and flag cases approaching LUPA thresholds. - Respond Quickly to Missed Visits:
If a patient cancels or misses a visit, reschedule immediately to avoid falling below the threshold. - Adjust as Needed:
Regularly review patient care plans during the billing cycle and make adjustments as necessary to stay on target. - Train Staff on LUPA Goals:
Educate clinicians and schedulers about the importance of LUPA thresholds and how they impact agency reimbursement. - Encourage Collaboration:
Maintain open communication between care coordinators, field staff, and administrators to ensure alignment. - Support Clinicians:
Provide field staff with tools to document visits accurately and report any issues in real time. - Audit LUPA Cases:
Analyze LUPA cases to identify trends and operational gaps that may be contributing factors. - Implement Best Practices:
Use findings from audits to develop and enforce improved processes for scheduling, documentation, and care delivery. - Continuously Improve:
Regularly assess staff feedback, patient outcomes, and operational data to optimize your LUPA prevention strategies.
The Bottom Line
Avoiding LUPA under PDGM is essential for maintaining financial stability, operational efficiency, and high-quality patient care. By focusing on accurate assessments, proper coding, strategic visit planning, and leveraging technology, agencies can effectively meet variable thresholds and prevent revenue losses.
Engaging patients, anticipating challenges, and fostering teamwork ensure a proactive approach that aligns with PDGM’s focus on value-driven care. Mastering LUPA management not only protects reimbursement but also enhances agency reputation, patient satisfaction, and long-term success. With the right strategies, your agency can thrive while delivering exceptional care.
ABOUT AUTHOR

Pedro Collins
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.