The healthcare industry is no stranger to artificial intelligence (AI). As the AI revolution sweeps across fields, it's no surprise that it's also making its mark in medical billing and coding. Yet, many providers and billing companies cling to traditional, manual methods, leading to inefficiencies that ultimately hurt their bottom line.
But here's the good news: AI isn't just a buzzword; it's a practical solution that's transforming the way healthcare practices handle their finances. In this guide, we'll explore how AI is revolutionizing medical billing and coding, easing the burden on healthcare professionals and paving the way for a more efficient future. So, grab a cup of coffee and let's dive in!
Why AI is Becoming Indispensable in Medical Billing and Coding?
Consider the sheer volume of data involved in medical billing: patient records, insurance claims, procedure codes, and ever-changing regulations. Manually managing this mountain of information is not only time-consuming but also prone to errors.
AI-powered solutions can sift through this data with lightning speed and accuracy, identifying discrepancies, flagging potential issues, and ensuring compliance with complex billing guidelines.
But AI's value goes beyond just data processing. It can also automate repetitive tasks like claim submission and denial management, freeing up human staff to focus on more complex and strategic aspects of their work. This not only boosts efficiency but also improves employee morale by eliminating the drudgery of mundane tasks.
Moreover, AI's ability to learn and adapt means it can continuously improve its performance over time, becoming even more adept at identifying patterns, predicting trends, and optimizing billing workflows. This translates to faster reimbursements, fewer denials, and ultimately, a healthier financial outlook for healthcare providers.
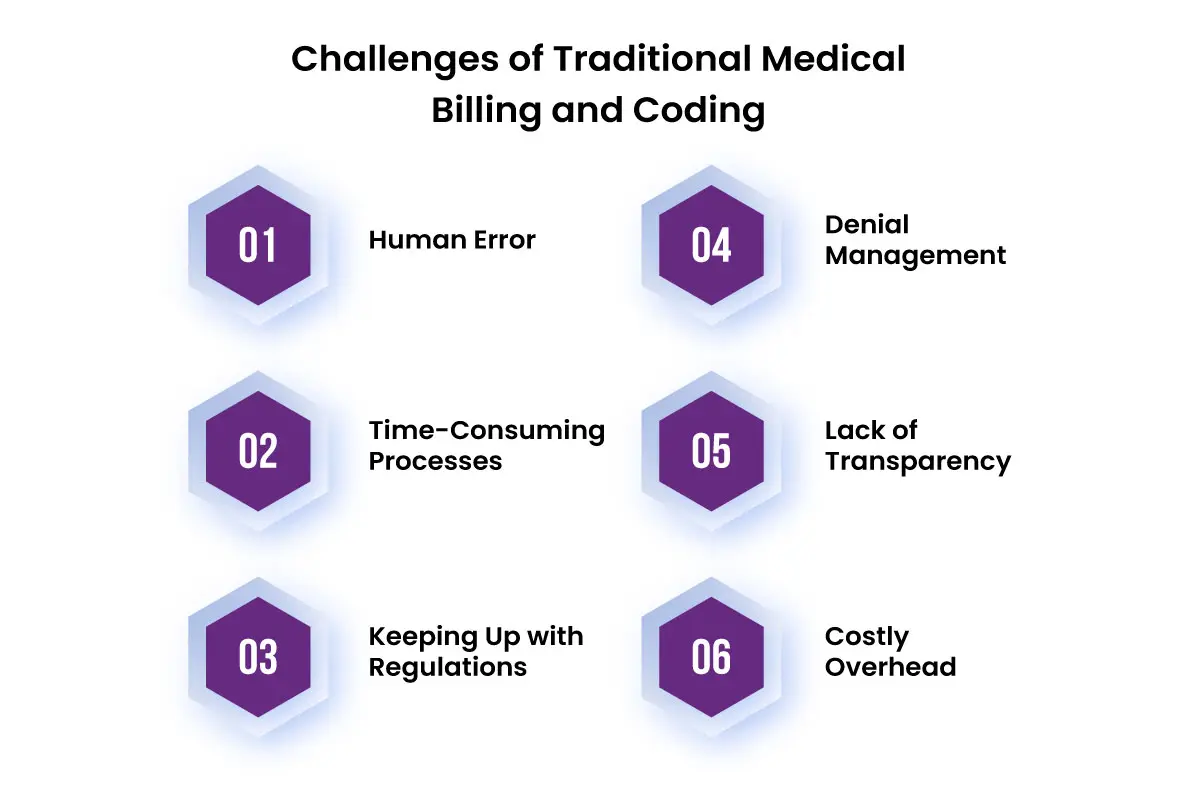
Challenges of Traditional Medical Billing and Coding
While traditional medical billing and coding processes have served the healthcare industry for years, they come with a unique set of challenges that can hinder efficiency, accuracy, and ultimately, revenue. Let's delve into some of these key issues:
-
Human Error: Manual data entry is a breeding ground for mistakes. From typos in patient information to incorrect procedure codes, these errors can lead to claim denials, delays in reimbursement, and even compliance issues. The sheer volume of data involved only amplifies the risk of human error.
-
Time-Consuming Processes: Medical billing and coding are complex and multi-step processes. Manually verifying patient eligibility, submitting claims, and tracking payments can be incredibly time-consuming, diverting valuable resources away from patient care.
-
Keeping Up with Regulations: The healthcare landscape is constantly evolving, with new regulations and coding guidelines emerging regularly. Staying abreast of these changes and ensuring compliance can be a daunting task for billing staff, especially when relying on manual methods.
-
Denial Management: Dealing with claim denials is a frustrating reality for many healthcare providers. Identifying the reason for denial, correcting the claim, and resubmitting it can be a lengthy and labor-intensive process, often resulting in delayed or lost revenue.
-
Lack of Transparency: Traditional billing processes often lack transparency, making it difficult for providers to track the status of claims, identify bottlenecks, and pinpoint areas for improvement. This lack of visibility can lead to inefficiencies and missed opportunities for optimization.
-
Costly Overhead: Maintaining a large billing staff, investing in training, and dealing with the fallout of errors all contribute to significant overhead costs for healthcare providers. These expenses can strain resources and impact the overall financial health of a practice.
These challenges highlight the need for a more efficient, accurate, and streamlined approach to medical billing and coding. Fortunately, AI-powered solutions offer a promising way to overcome these hurdles and transform the way healthcare practices manage their revenue cycle.
Comparing AI Medical Coding With Human Coding
While both AI and human medical coders aim for accurate and efficient billing, their approaches and strengths differ significantly.
|
Feature |
AI Medical Coding |
Human Medical Coding |
|
Speed |
Processes vast amounts of data in seconds. |
Takes significantly longer, especially with complex cases. |
|
Accuracy |
High accuracy due to pattern recognition and data analysis. |
Prone to human error, especially with fatigue or distraction. |
|
Consistency |
Maintains consistent coding standards across all claims. |
Can vary depending on individual coder's expertise and judgment. |
|
Learning |
Continuously learns and improves through machine learning. |
Requires ongoing training to stay updated with new guidelines. |
|
Cost |
Potentially more cost-effective in the long run due to automation. |
High labor costs due to manual processes and training needs. |
|
Complexity |
Can handle repetitive tasks and large volumes of data easily. |
Better suited for complex cases requiring nuanced interpretation. |
|
Adaptability |
Quickly adapts to new coding guidelines and regulations. |
May take time to adjust to changes and require additional training. |
|
Creativity |
Lacks creativity and critical thinking for complex scenarios. |
Can apply creative problem-solving to ambiguous cases. |
How is AI Serving Billers and Coders?
AI is proving to be a game-changer in the realm of medical billing and coding, offering innovative solutions that streamline processes, improve accuracy, and ultimately, enhance revenue cycle management.
Billers
-
Automated Claim Processing: AI-powered software can automatically extract relevant data from medical records, populate claim forms, and submit them electronically, significantly reducing manual effort and the risk of errors.
-
Intelligent Denial Management: AI algorithms can analyze denied claims, identify the root causes, and suggest corrective actions, leading to faster resubmission and improved reimbursement rates.
-
Predictive Analytics: By analyzing historical billing data, AI can identify patterns and trends, predict potential denials, and recommend proactive measures to prevent them.
-
Payment Posting Automation: AI can streamline the process of matching payments to invoices, reducing manual reconciliation efforts and ensuring accurate financial records.
-
Fraud Detection: AI algorithms can detect suspicious billing patterns and potential fraud, safeguarding the financial integrity of healthcare practices.
Coders
For medical coders, AI serves as a knowledgeable assistant, helping them navigate the complex world of medical codes with greater speed and accuracy. Here's how:
-
Computer-Assisted Coding (CAC): AI-powered CAC tools can suggest appropriate codes based on clinical documentation, reducing manual coding time and minimizing errors.
-
Natural Language Processing (NLP): NLP algorithms can extract relevant information from unstructured clinical notes, streamlining the coding process and improving accuracy.
-
Clinical Documentation Improvement (CDI): AI can analyze clinical documentation and identify opportunities for improvement, ensuring accurate and complete coding that supports optimal reimbursement.
-
Medical Coding Audits: AI can automatically audit coded charts, identifying potential errors and inconsistencies, helping coders maintain high levels of accuracy and compliance.
-
Continuous Learning: AI algorithms can continuously learn from feedback and new data, improving their coding accuracy and staying up-to-date with the latest coding guidelines.
Future of AI in Healthcare Billing
The current applications of AI in medical billing and coding are just the tip of the iceberg. As technology continues to evolve at a breakneck pace, the future holds even more exciting possibilities.
Hyper-Automation:
AI will go beyond automating individual tasks to orchestrating entire billing workflows. This will lead to unprecedented efficiency, accuracy, and speed in processing claims, resulting in faster reimbursements and improved cash flow for healthcare providers.
Advanced Analytics:
AI-powered analytics will unlock deeper insights into billing patterns, denial trends, and revenue cycle performance. This data-driven approach will empower healthcare organizations to make informed decisions, optimize processes, and identify opportunities for growth.
Personalized Patient Engagement:
AI-powered chatbots and virtual assistants will revolutionize patient communication, offering personalized support for billing inquiries, payment options, and financial assistance programs. This will improve patient satisfaction and reduce the burden on billing staff.
Predictive Modeling:
AI will leverage machine learning to predict claim denials, identify potential coding errors, and forecast revenue trends. This proactive approach will enable healthcare providers to address issues before they escalate, minimizing revenue loss and maximizing financial performance.
Integration with Electronic Health Records (EHRs):
AI will seamlessly integrate with EHRs, extracting relevant data for billing and coding purposes, minimizing manual data entry, and ensuring accurate and complete documentation.
Enhanced Cybersecurity:
As healthcare data becomes increasingly valuable, AI will play a crucial role in safeguarding sensitive patient information. AI-powered cybersecurity tools will detect and prevent fraud, ensuring the integrity and confidentiality of medical billing data.
Bottom Line
The bottom line is clear: AI is not just a passing trend in medical billing and coding; it's a game-changing force that's here to stay. Embracing this technology isn't just about keeping up with the times; it's about empowering your practice to thrive in an increasingly complex healthcare landscape.
While the road to AI adoption may have its curves, the rewards far outweigh the challenges. So, don't be left behind. Embrace the AI revolution and empower your practice to thrive in the digital age of healthcare.
ABOUT AUTHOR

John Wick
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.
