Healthcare is built on precision—not just in patient care but in the way that care is documented. Each note, diagnosis, and treatment recorded in a patient’s medical chart holds weight, influencing outcomes far beyond the bedside.
But what happens when those records don’t fully capture the complexity of a patient’s condition? Clinical Documentation Improvement (CDI) is the solution, ensuring that every aspect of care is accurately reflected, from diagnosis to billing.
Whether you’re a healthcare professional or someone curious about the mechanics behind patient records, understanding CDI is essential to appreciating how healthcare works seamlessly. Let’s take a closer look at why CDI matters and how it shapes the future of care delivery.
What is CDI in Healthcare?
Clinical Documentation Improvement (CDI) is the process of making sure that a patient’s medical records are clear, complete, and accurate. It ensures that every detail about a patient’s diagnosis, treatment, and care is properly documented. This isn’t just about paperwork—it’s about reflecting the true story of the patient’s health.
Good documentation is essential for many reasons. It helps doctors and nurses provide better care, supports coders in assigning correct medical codes for billing, and ensures healthcare providers get reimbursed properly by insurance companies. CDI specialists work closely with doctors, nurses, and coders to review records, ask questions when something is unclear, and improve the overall quality of documentation.
In simple terms, CDI helps translate the care a patient receives into an accurate medical record, making sure nothing is left out or misunderstood.
The Origin of CDI Programs
Clinical Documentation Improvement (CDI) programs trace their roots back to 1983 when the Centers for Medicare and Medicaid Services (CMS) introduced the Diagnostic-Related Group (DRG) system. This revolutionary system redefined hospital reimbursement, tying payments to the severity of a patient’s condition and the complexity of care provided.
To ensure proper reimbursement under this new model, healthcare organizations recognized the need for accurate and detailed clinical documentation. CDI programs were developed as a solution, focusing on improving the quality and completeness of medical records to reflect the true nature of patient care.
Initially centered around hospital-based reimbursement, CDI has since evolved into a cornerstone of healthcare operations, supporting accurate coding, compliance, and better patient care across diverse settings.
Impact of Clinical Documentation Improvement (CDI) in the Inpatient Setting
Clinical Documentation Improvement (CDI) has had a profound and transformative impact on inpatient care, influencing various aspects of healthcare delivery, from patient outcomes to operational efficiency and financial integrity.
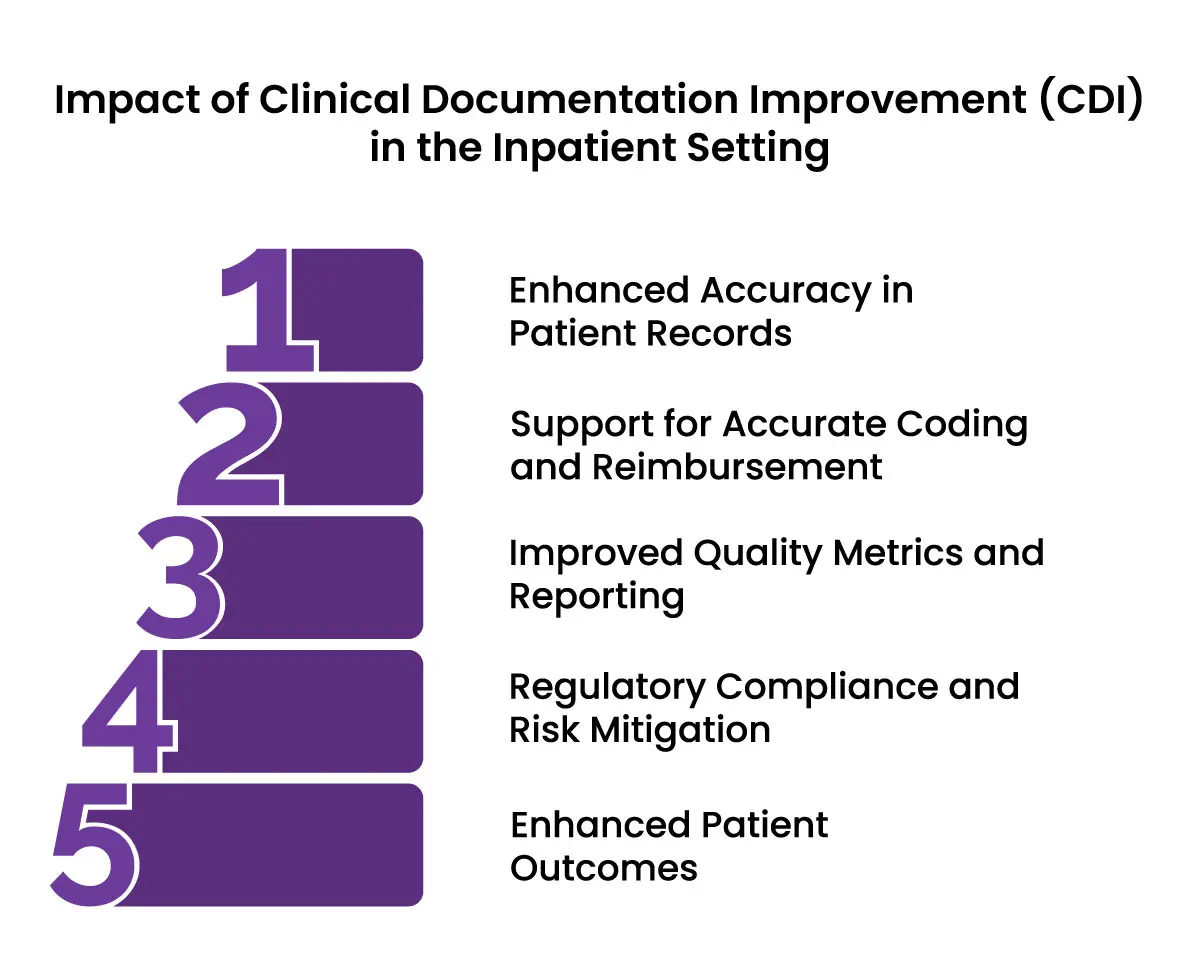
1. Enhanced Accuracy in Patient Records
In the inpatient setting, patient care often involves complex diagnoses, comorbidities, and multi-disciplinary treatments. CDI ensures that medical records accurately reflect the full scope of a patient’s health status. This level of detail:
-
Facilitates continuity of care: Precise documentation helps healthcare providers understand a patient’s history and current status, enabling informed clinical decisions.
-
Improves communication: Accurate records ensure that all members of the care team are on the same page, reducing errors and miscommunication.
2. Support for Accurate Coding and Reimbursement
One of the core objectives of CDI is to align clinical documentation with coding standards, particularly for the ICD-10 system. In an inpatient setting:
-
Appropriate reimbursement: Accurate documentation ensures that hospitals receive fair payment for the level of care provided. For example, proper identification and recording of complications or comorbid conditions (CCs) and major complications or comorbid conditions (MCCs) directly impact the Diagnosis-Related Group (DRG) assignments, which determine reimbursement rates.
-
Reduction of claim denials: Incomplete or unclear documentation can lead to coding errors and subsequent claim denials. CDI programs reduce this risk by addressing gaps in documentation upfront.
3. Improved Quality Metrics and Reporting
Inpatient hospitals are evaluated on numerous quality measures, many of which rely on the accuracy of clinical documentation. CDI impacts:
-
Hospital quality scores: Metrics such as mortality rates, readmission rates, and complication rates are directly linked to documentation accuracy. CDI helps ensure these metrics are reflective of the true clinical picture.
-
Value-based purchasing (VBP): Under CMS’s VBP program, hospitals are rewarded or penalized based on their performance metrics. CDI supports better scores by ensuring that documentation captures all conditions affecting patient care.
-
Public reporting: Accurate documentation influences data that is shared publicly, such as hospital rankings, and helps maintain a hospital’s reputation.
4. Regulatory Compliance and Risk Mitigation
In the inpatient setting, compliance with regulatory requirements is critical. CDI ensures:
-
Adherence to CMS guidelines: By improving documentation accuracy, hospitals can meet the standards set by CMS and other regulatory bodies.
-
Audits and reviews: Proper documentation minimizes the risk of negative outcomes during audits by recovery audit contractors (RACs) or other oversight entities.
-
Legal protection: Comprehensive records provide a clear picture of the care provided, reducing liability risks in case of legal scrutiny.
5. Enhanced Patient Outcomes
CDI indirectly improves patient outcomes by promoting a culture of precision and accountability. In the inpatient setting:
-
Accurate diagnoses: Improved documentation ensures that conditions are identified and treated appropriately, avoiding missed or delayed diagnoses.
-
Better care planning: Detailed records help providers create effective care plans, particularly for patients with multiple or chronic conditions.
-
Reduced readmissions: By documenting and addressing all relevant conditions during the initial admission, hospitals can reduce the likelihood of readmissions.
The Role of CDI in Preventing Overbilling and Ensuring Accurate Diagnoses
Inaccurate clinical documentation can lead to significant consequences for healthcare facilities, as demonstrated in a July 2020 Office of Inspector General (OIG) audit. The audit revealed that hospitals overbilled Medicare by $1 billion due to incorrectly assigning severe malnutrition diagnosis codes on inpatient claims. Of the 200 claims reviewed, 164 were found to have improper coding, where severe malnutrition was documented but should have been classified as another form of malnutrition—or no malnutrition at all.
The fallout from this audit was substantial, with the OIG recommending Medicare recoup overpayments from providers where possible. This situation highlights the critical need for robust Clinical Documentation Improvement (CDI) programs to prevent such errors.
How a CDI Specialist Improves the Accuracy of Claims Being Submitted
The accuracy of claims submitted by healthcare facilities directly hinges on the quality and completeness of the clinical documentation supporting them. A Clinical Documentation Improvement (CDI) specialist plays a pivotal role in bridging the gap between clinical care and billing accuracy.
Ensuring Documentation Reflects Clinical Reality
One of the key responsibilities of a CDI specialist is to align the documentation in medical records with the actual clinical presentation of the patient. They meticulously review inpatient or outpatient records to confirm that all diagnoses, procedures, and treatments are documented in a manner that reflects the complexity and severity of the case. This ensures that nothing significant is overlooked, and every condition impacting care is clearly described.
For example, if a patient with pneumonia also has underlying chronic obstructive pulmonary disease (COPD), a CDI specialist ensures that both conditions are documented. This level of detail is critical for accurate coding and appropriate claim submission.
Clarifying Ambiguities Through Provider Queries
When documentation lacks clarity or is incomplete, CDI specialists step in to seek clarification from providers. They issue detailed and compliant queries to physicians, asking for additional information or requesting specificity. Queries might focus on confirming a diagnosis, clarifying the clinical significance of a finding, or ensuring the inclusion of comorbid conditions.
For instance, if a provider documents "malnutrition" without specifying the severity (mild, moderate, or severe), the CDI specialist will query the provider to accurately capture the severity based on clinical criteria such as lab values or weight loss. This precision is essential for proper code assignment and reimbursement.
Aligning Documentation with Coding Standards
CDI specialists ensure that documentation meets the specific requirements of coding systems, such as ICD-10-CM and ICD-10-PCS. Coding relies on the specificity and accuracy of the documentation to assign codes that directly impact Diagnosis-Related Groups (DRGs) in inpatient settings.
For example, a vague diagnosis like "kidney failure" needs to be clarified to specify whether it is acute or chronic, with or without complications. By ensuring the documentation is detailed and specific, CDI specialists help coders assign the most accurate and compliant codes.
Integrating Technology for Real-Time Improvements
CDI specialists leverage advanced tools like Clinical Decision Support (CDS) systems and natural language processing (NLP) software to identify documentation gaps in real-time. These technologies flag incomplete or inconsistent documentation, enabling CDI specialists to address issues while the patient is still in care. This proactive approach ensures that claims are supported by thorough and accurate records from the outset.
How CDI Can Impact Patient Care
Clinical Documentation Improvement (CDI) directly impacts patient care by ensuring medical records accurately reflect the full scope of a patient’s health status and care needs. This clarity supports better diagnoses, more tailored treatment plans, and improved care coordination across providers.
CDI also plays a critical role in enhancing continuity of care, particularly during transitions between care settings, by ensuring comprehensive documentation for handoffs. Additionally, it helps reduce readmissions by addressing gaps in discharge planning and outpatient care instructions.
Through accurate documentation, CDI contributes to quality reporting and supports fair risk adjustment, which is essential for programs like the Hospital Readmissions Reduction Program (HRRP). By capturing all relevant comorbidities and complexities, hospitals can avoid penalties under HRRP, which penalizes facilities for higher-than-expected readmission rates.
CDI’s impact extends to improving patient safety, minimizing documentation errors, and empowering providers through education on best practices. It ensures documentation is specific and compliant with coding standards, reducing risks tied to claim denials and financial penalties.
Furthermore, CDI programs enhance the accuracy of quality metrics, enabling healthcare organizations to improve public reporting and maintain fair reimbursement. By focusing on complete, accurate, and actionable documentation, CDI strengthens patient care while aligning with regulatory and financial objectives like those addressed by HRRP.
Comparing the CDI Process Inpatient vs. Outpatient Settings
|
Aspect |
Inpatient CDI |
Outpatient CDI |
|
Focus Area |
Acute conditions, comorbidities, and severity of illness |
Chronic condition management, preventive care, and risk adjustment |
|
Documentation Timing |
Concurrent reviews during hospitalization |
Retrospective reviews post-visit |
|
Primary Coding System |
ICD-10-CM/PCS and DRG assignment |
ICD-10-CM and HCC coding |
|
Reimbursement Model |
Fee-for-service with DRG-based reimbursement |
Value-based care and risk adjustment models |
|
Quality Metrics |
Mortality rates, readmission rates, and HRRP compliance |
Risk adjustment factor (RAF) scores and preventive care metrics |
|
Common Challenges |
Capturing complex diagnoses, ensuring DRG accuracy |
Documenting chronic conditions, ensuring E/M coding accuracy |
Final Words
Clinical Documentation Improvement (CDI) serves as the backbone of effective healthcare management, ensuring that patient records are not only precise but also capture the true complexity of care delivered. By enhancing the accuracy of documentation, CDI bridges the gap between clinical care and administrative processes, driving improved outcomes across the board.
It enables seamless communication, reduces the risk of claim denials, and supports compliance with regulatory measures such as HRRP, protecting providers from penalties. At its core, CDI is a powerful tool that safeguards financial integrity, enhances patient safety, and ensures healthcare systems operate with clarity and accountability. In an ever-evolving landscape, CDI remains a critical driver of quality, transparency, and trust in care delivery.
ABOUT AUTHOR

Pedro Collins
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.