In modern healthcare, the synergy between Chronic Care Management (CCM) and Current Procedural Terminology (CPT) codes is integral to providing comprehensive and uninterrupted care. As healthcare professionals strive to optimize patient outcomes, CCM emerges as a strategic approach, offering continuous support for individuals grappling with chronic conditions.
Complementing this care model, CPT codes serve as the standardized language, allowing practitioners to effectively communicate, document, and ensure accurate reimbursement for the vital services rendered.
This guide aims to illuminate the symbiotic relationship between CCM and CPT codes, offering insights into their roles and implications within the dynamic landscape of healthcare provision.
What is Chronic Care Management?
Chronic Care Management (CCM) is a tailored healthcare strategy designed for individuals grappling with chronic conditions. Unlike traditional care models, CCM emphasizes continuous and personalized support, aiming to optimize patient outcomes and minimize healthcare costs through early intervention.
This proactive approach involves a collaborative healthcare team working together to create customized care plans addressing individual patient needs. By prioritizing preventive measures, CCM not only enhances the overall quality of life for patients but also reduces the frequency of hospitalizations. Incorporating CCM into healthcare practices fosters a patient-centric approach, effectively managing the challenges posed by chronic health conditions and promoting overall well-being.
What Are CPT Codes for Chronic Care Management?
CPT codes for Chronic Care Management (CCM) provide a structured framework for healthcare providers to bill and document essential services for individuals with chronic medical conditions. These codes play a pivotal role in facilitating seamless communication, documentation, and reimbursement processes.
Here are the key CPT codes for Chronic Care Management:
Non-Complex CCM:
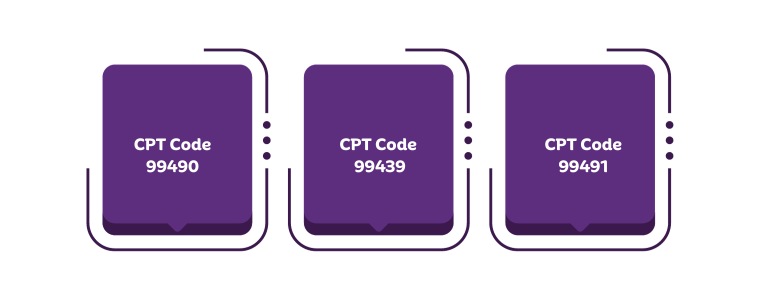
CPT Code 99490: Clinical staff offers a 20-minute timed service, ensuring seamless care coordination across providers while fostering patient accountability.
CPT Code 99439: Additional 20-minute increments of clinical staff time, directed by a physician or qualified healthcare professional, complementing non-complex CCM. Billed alongside CPT code 99490.
CPT Code 99491: Physicians or qualified healthcare professionals personally provide CCM services for a minimum of 30 minutes, ensuring personalized care for patients.
Complex CCM:
CPT Code 99487: Involving a 60-minute timed service by clinical staff, complex CCM substantially revises or establishes comprehensive care plans, showcasing expertise in moderate- to high-complexity medical decision-making.0
CPT Code 99489: Each additional 30 minutes of clinical staff time for complex CCM, directed by a physician or qualified healthcare professional. This code is reported in conjunction with CPT code 99487 and cannot be billed with CPT code 99490.
Below is the table summarizing the above information
| CPT Code | Description | Duration | Reimbursement Rate |
| 99490 | Non-Complex CCM | 20 mins | $62.69 |
| 99439 | Additional 20 mins (Non-Complex CCM) | 20 mins |
$47.44 |
| 99491 | Personalized CCM by Physicians or Qualified Healthcare Professionals | 30 mins | $85.06 |
| 99487 | Complex CCM | 60 mins | $133.18 |
| 99489 | Additional 30 mins (Complex CCM) | 30 mins | $70.49 |
CCM CPT codes herald a future of accessibility, connectivity, and cost-effective care. Through collaboration and innovation, these codes illuminate a path toward improved well-being, ensuring a brighter future for healthcare.
Importance of CPT Codes For Chronic Care Management
Ensuring effective Chronic Care Management (CCM) is crucial in enhancing patient outcomes and streamlining healthcare processes. The use of Current Procedural Terminology (CPT) codes plays a pivotal role in this domain, offering a standardized system for documenting and billing for various aspects of chronic care services.
Accurate Reimbursement: CPT codes provide a precise framework for healthcare providers to document and bill for the diverse services involved in chronic care management, ensuring accurate and fair reimbursement.
Transparent Communication: These codes serve as a common language between healthcare professionals, payers, and regulators, facilitating transparent communication regarding the specific services provided and the associated costs.
Streamlined Documentation: CPT codes contribute to organized and standardized documentation of chronic care services, enabling efficient record-keeping and enhancing communication among healthcare team members.
Optimized Care Planning: The use of CPT codes allows for a systematic approach to care planning, ensuring that healthcare providers can tailor their services to the unique needs of patients with chronic conditions.
In summary, CPT codes are integral to the effective functioning of Chronic Care Management. They provide a standardized and transparent way to document, communicate, and bill for the various aspects of care, ultimately contributing to improved patient outcomes and the overall efficiency of healthcare delivery.
The Benefits of Utilizing CPT Codes in Chronic Care Management
Effectively managing chronic care requires a structured approach, and the utilization of Current Procedural Terminology (CPT) codes proves instrumental in achieving this goal. The benefits of incorporating CPT codes into chronic care management are diverse and impactful.
-
Increase Revenue
-
Improved Patient Outcomes
-
Enhance Patient Satisfaction
-
Better Care Coordination
Incorporating CPT codes into chronic care management stands as a key practice, ensuring efficiency, transparency, and improved patient outcomes. This structured system not only elevates the overall quality of care but also contributes to the financial well-being of healthcare practices, fostering a comprehensive and patient-centric approach to chronic care.
Integrate CCM Software in Chronic Care Management
Integrating CCM software into chronic care management is a game-changer, streamlining healthcare processes for more efficient patient care. This advanced tool provides healthcare professionals with a centralized platform for effective communication, streamlined documentation, and accurate billing, optimizing the overall workflow seamlessly.
Beyond operational benefits, CCM software transforms the patient experience. It enables personalized care plans, enhances patient engagement, and fosters improved communication between healthcare providers and their patients. The integration not only elevates the standard of care but also contributes to increased patient satisfaction and better health outcomes.
Billing and Coding Guidelines for Chronic Care Management
Navigating the complexities of billing and coding in Chronic Care Management (CCM) requires a comprehensive understanding of guidelines to ensure accurate reimbursement and compliance with Centers for Medicare & Medicaid Services (CMS) standards.
Here are some essential tips:
Accurate Code Application: Ensure proper application of CPT codes for each program managed, linking them to corresponding ICD-10 codes for the conditions within those programs.
Detailing Date and Place of Service: Include the specific date and place of service for each encounter, with a common scenario being in-office or telehealth settings.
National Provider Identifier (NPI) Inclusion: Include your National Provider Identifier (NPI) number on all submitted claims for proper identification.
Record Care Manager Information: While not mandatory, noting the assigned care manager in your records can be beneficial in case of an audit.
To successfully bill for CCM services, follow these steps:
Monthly CMS Verification: Ensure all CMS requirements are met for each patient monthly.
Monthly Claims Submission: Submit claims to CMS monthly for timely reimbursement.
Invoice Patients: Provide invoices to patients receiving monthly CCM services, maintaining transparency in billing practices.
Code Conflict Resolution: Verify there are no conflicting codes that have been billed, ensuring accuracy and compliance.
Effective billing and coding practices not only secure proper reimbursement but also contribute to the overall success of Chronic Care Management, optimizing patient care and organizational efficiency.
Final Thoughts
In the dynamic field of Chronic Care Management, a clear grasp of billing and coding guidelines is essential. Accurate application of CPT and ICD-10 codes ensures compliance with CMS standards, promoting effective reimbursement. Details such as the date, place of service, and NPI numbers add precision, with the knowledge of the assigned care manager proving valuable during audits.
Implementing these guidelines ensures a seamless billing process, securing accurate reimbursement and establishing transparency in financial interactions with patients. From monthly verifications to timely claims submissions and resolution of potential code conflicts, these practices enhance the overall efficiency of CCM services. Embracing sound billing and coding practices in Chronic Care Management is foundational, fostering a sustainable and patient-centric approach in the ever-evolving landscape of healthcare.
ABOUT AUTHOR

Abeed Hossain
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.