The CLIA of 1988 established a federal framework regulating laboratory testing on human specimens for health purposes. For healthcare facilities like physician's offices, urgent care centers, and others, understanding CLIA requirements is crucial for both regulatory compliance and ensuring proper medical billing and reimbursement.
What is CLIA?
The Clinical Laboratory Improvement Amendments (CLIA) were established in 1988 to ensure quality laboratory testing across the United States. Regulated by the Centers for Medicare & Medicaid Services (CMS), CLIA applies to all facilities that perform tests on human specimens for health assessment or to diagnose, prevent, or treat disease.
CLIA Certification Types
There are several types of CLIA certificates based on the complexity of testing performed:
-
Certificate of Waiver (CoW) - For laboratories performing only waived tests
-
Certificate for Provider-Performed Microscopy Procedures (PPMP) - For labs performing waived tests plus specific microscopy procedures
-
Certificate of Compliance (CoC) - For labs performing moderate and/or high complexity tests that undergo routine inspections
-
Certificate of Accreditation (CoA) - For labs performing moderate and/or high complexity tests accredited by an approved organization
-
Certificate of Registration (CoR) - A temporary certificate issued until determinations of compliance can be made
For many medical practices, the Certificate of Waiver is the most common and straightforward option.
CLIA Waiver Requirements
To qualify for a CLIA waiver, your facility must:
-
Perform only waived tests that are simple with minimal risk of error
-
Follow manufacturers' instructions for all waived tests
-
Pay the applicable certificate fee
-
Allow on-site inspections when requested by CMS
-
Notify your state agency about changes in ownership, name, address, or test menu
-
Maintain records of testing for at least two years
How to Apply for a CLIA Waiver
Obtaining a Certificate of Waiver involves these steps:
-
Complete Form CMS-116: The "Clinical Laboratory Improvement Amendments (CLIA) Application for Certification"
-
Submit to State Agency: Send the completed application to your state's Department of Health CLIA program
-
Pay the Fee: The current fee for a Certificate of Waiver is $180 for two years
-
Receive Your Certificate: Once approved, you'll receive a certificate valid for two years
The application requires information about your facility, director, ownership, testing personnel, and the specific tests you'll perform.
CLIA Number for Medical Billing
A CLIA number (also called a CLIA ID) is a unique 10-character identifier assigned to your laboratory upon certification. This number is crucial for medical billing purposes as it must be included on claims for laboratory services submitted to Medicare and many other insurers.
The format typically follows this pattern:
-
First two characters: State code
-
Next two digits: Number representing the certificate type
-
Remaining characters: Unique identifier for the laboratory
CLIA Waived Tests List
The FDA maintains an updated list of CLIA-waived tests. Some common waived tests include:
-
Blood glucose monitoring
-
Hemoglobin A1C
-
Urine pregnancy tests
-
Rapid strep tests
-
Fecal occult blood tests
-
Influenza A/B rapid tests
-
COVID-19 rapid antigen tests
-
Cholesterol screening
-
Prothrombin time/INR
-
H. pylori antibody tests
The full list is extensive and continually updated as new tests receive waived status. The CDC maintains a comprehensive document listing all tests granted waived status, which can be accessed through their website.
CLIA Waiver CPT Codes
When billing for CLIA-waived tests, you must use the appropriate CPT codes along with the QW modifier, which specifically indicates the test is CLIA-waived. Some common CLIA-waived test CPT codes include:
-
82962-QW: Glucose monitoring by glucose meter
-
83036-QW: Hemoglobin A1C test
-
81002-QW: Urinalysis, non-automated without microscopy
-
87880-QW: Strep A, direct optical observation
-
85610-QW: Prothrombin time (PT)
-
82270-QW: Blood occult, feces screening
It's important to note that without the QW modifier, many claims for these laboratory tests will be denied by Medicare and other payers.
Billing for CLIA Waived Tests
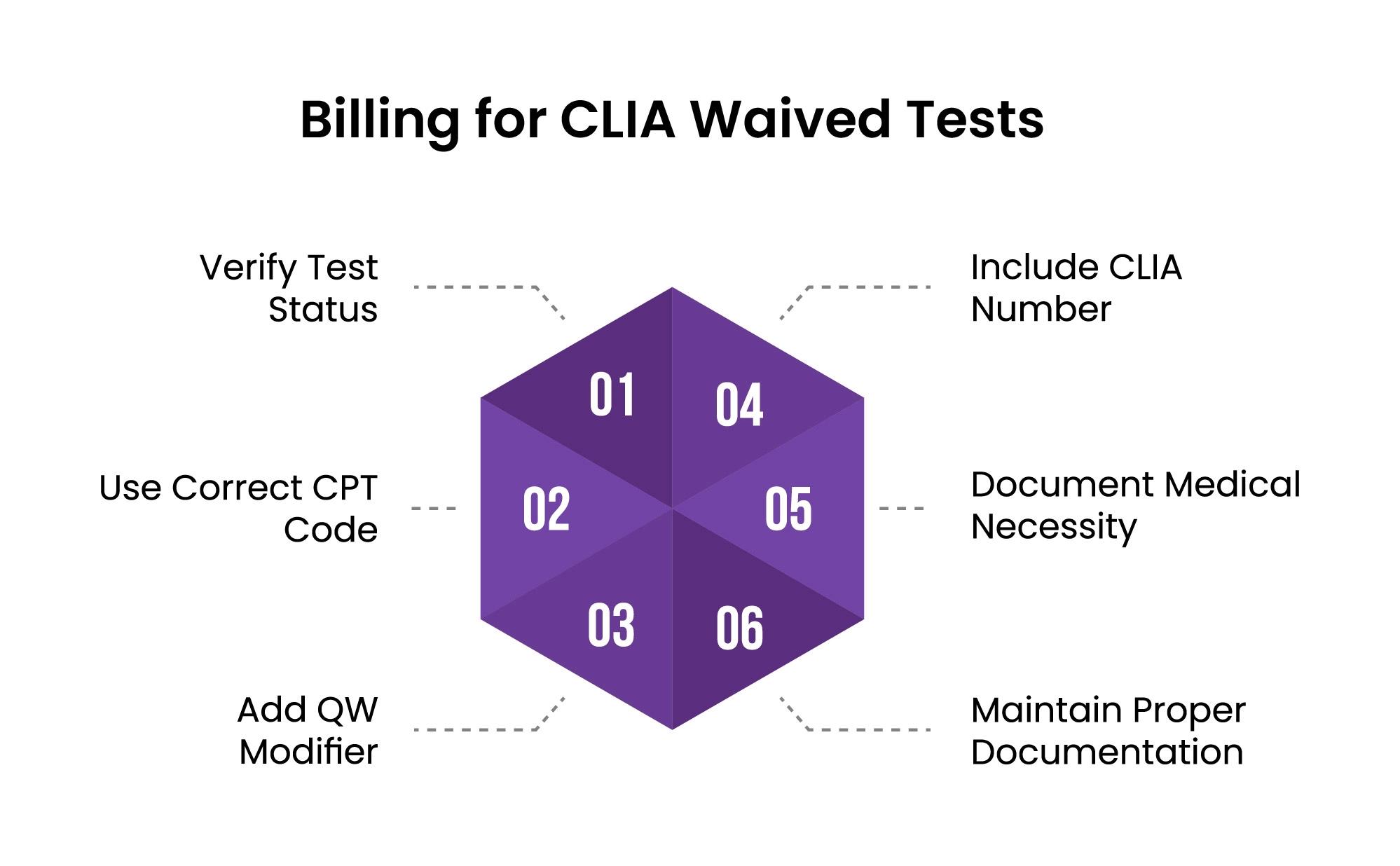
1. Verify Test Status
Before billing for any laboratory test as CLIA-waived, you must confirm its official classification on the FDA's CLIA waived test list. This verification is critical because:
-
Test classifications can change over time as manufacturers update methodologies
-
Some tests may appear similar but have different complexity classifications
-
Performing or billing for tests beyond your certificate's scope violates CLIA regulations
You can verify a test's waived status through:
-
The FDA's CLIA Database (accessible via their website)
-
The test manufacturer's package insert which explicitly states the CLIA classification
-
The CDC's comprehensive list of tests granted waived status (updated quarterly)
If a test is not officially classified as waived, billing it with a QW modifier would constitute improper billing and could trigger an audit.
2. Use Correct CPT Code
Each laboratory test has specific CPT (Current Procedural Terminology) codes assigned by the American Medical Association that identify the precise procedure performed:
-
CPT codes are five-digit numeric codes (e.g., 82962 for glucose blood testing)
-
Tests may have multiple CPT code options depending on methodology used
-
The correct code must reflect the exact methodology of the test performed
-
Using an incorrect or less specific code may result in improper reimbursement or denials
For example, a rapid strep test might use code 87880 (Streptococcus, group A, direct optical observation), but if you performed a culture instead, a different code would be required, even though both test for strep.
3. Add QW Modifier
The QW modifier is a critical two-character code specifically created by CMS to identify CLIA-waived tests:
-
It must be appended directly to the CPT code (e.g., 87880-QW)
-
The modifier tells the payer that:
-
The test is officially classified as CLIA-waived
-
Your facility is appropriately certified to perform it
-
The simplified methodology justifies a potentially different reimbursement rate
-
-
Without the QW modifier, claims processing systems may:
-
Automatically reject the claim
-
Flag it for manual review, delaying payment
-
Apply incorrect reimbursement rates
-
Medicare and many commercial payers will automatically deny laboratory claims for waived tests if the QW modifier is missing, even if the facility has the appropriate CLIA certificate.
4. Include CLIA Number
Your CLIA identification number is a mandatory identifier that proves your laboratory's certification status:
-
For paper claims using CMS-1500 forms:
-
Enter the 10-digit CLIA number in Box 23 (labeled "Prior Authorization Number")
-
The entire number must be clearly legible
-
If multiple laboratories performed different tests on the same claim, you may need to submit separate claim forms
-
-
For electronic claims (ANSI X12 837P format):
-
Include in Loop 2300, REF segment
-
REF01 = "X4" (CLIA indicator)
-
REF02 = your 10-digit CLIA number
-
Your clearinghouse or billing software vendor can provide specific instructions for your system
-
-
Common claim rejection reasons related to CLIA numbers include:
-
Missing CLIA number
-
Expired certificate at time of service
-
Mismatch between CLIA number and performing provider
-
Certificate type doesn't cover the procedure billed
-
5. Document Medical Necessity
Medical necessity documentation creates the clinical justification for performing the test:
-
Each test must be linked to a specific ICD-10 diagnosis code that supports the need for testing
-
The diagnosis must demonstrate why the test was reasonable and necessary
-
Documentation should include:
-
Patient symptoms or condition requiring diagnosis/monitoring
-
How test results will influence treatment decisions
-
Compliance with frequency limitations (some tests have restrictions on how often they can be performed)
-
Medicare and other payers maintain lists of "covered diagnoses" for certain laboratory tests through National Coverage Determinations (NCDs) and Local Coverage Determinations (LCDs). For example:
-
HbA1C testing (83036-QW) requires diabetes-related diagnosis codes
-
Lipid panel testing (80061-QW) requires cardiovascular risk or monitoring diagnoses
-
Pregnancy testing requires symptoms or conditions warranting confirmation of pregnancy
6. Maintain Proper Documentation
Comprehensive documentation is essential both for compliance and in case of audit:
-
Test requisition documentation should include:
-
Specific test ordered (not just "labs")
-
Ordering provider's signature
-
Date of order
-
Clinical indication/diagnosis
-
-
Testing documentation should include:
-
Date and time of specimen collection
-
Date and time of test performance
-
Identity of person performing the test
-
Test methodology used
-
Quality control results
-
Test results with appropriate reference ranges
-
Result interpretation when applicable
-
Additional records to maintain:
-
Equipment maintenance logs
-
Temperature logs for reagent storage
-
Staff training documentation
-
Manufacturer's package inserts for all test systems
-
Lot numbers and expiration dates of testing supplies
Proper documentation serves multiple purposes:
-
Demonstrates regulatory compliance with CLIA requirements
-
Supports the medical necessity of testing for reimbursement
-
Provides evidence in case of payer audits
-
Creates legal protection in case of disputed results
-
Facilitates quality improvement initiatives
CLIA Compliance for Providers
Healthcare providers must maintain ongoing CLIA compliance by:
-
Performing Only Authorized Tests: Stay within the scope of your certificate
-
Following Test Instructions: Adhere to manufacturers' guidelines precisely
-
Training Personnel: Ensure all staff are properly trained
-
Quality Control: Implement quality control procedures as required
-
Certificate Renewal: Renew your CLIA certificate every two years
-
Notifying Changes: Report any significant changes in your facility or testing menu
-
Documentation: Maintain thorough records of all testing procedures, results, and quality control measures
CLIA Requirements for Physician Offices
Physician offices face specific CLIA considerations:
-
Provider-Performed Microscopy: Physicians who want to perform certain microscopy procedures need a PPMP certificate instead of a basic waiver
-
Multiple Locations: Each physical location where testing occurs needs its own CLIA certificate
-
Medical Director: A qualified physician must serve as the laboratory director
-
Staff Competency: Regular assessment of staff competency is required
-
Test Selection: Carefully consider which tests to perform in-house versus sending to reference labs
Conclusion
CLIA waivers represent an important regulatory framework that ensures quality laboratory testing while allowing healthcare providers to perform simple diagnostic tests in-house. Understanding the requirements for obtaining and maintaining a CLIA Certificate of Waiver—along with proper billing procedures—is essential for healthcare practices seeking to optimize their laboratory services.
By following the guidelines outlined in this article, you can ensure your practice remains compliant with CLIA regulations while maximizing appropriate reimbursement for the laboratory services you provide.
ABOUT AUTHOR

Alex White
I’m Alex White, a Senior A/R Specialist with years of experience in medical billing and coding. I specialize in revenue cycle management and reimbursement processes, with a passion for accuracy and efficiency. Through my writing, I aim to share valuable insights and be a trusted voice in the medical billing and coding industry.