Denials are a constant challenge when it comes to managing your practice’s revenue cycle. Whether you’ve faced a number of them already or just started seeing claims rejected, one denial that can be particularly frustrating is CO 11—the dreaded “Diagnosis and Procedure Mismatch.”
There may be scenarios where you had a claim returned with this denial code. This common issue can stall your reimbursement process and create additional administrative headaches. In this blog, we’ll break down what CO 11 means, why it happens, and what you can do to resolve it quickly and efficiently.
What Does Denial Code 11 Mean?
Denial Code 11, also known as "Diagnosis and Procedure Mismatch", occurs when there is an inconsistency between the diagnosis code (ICD code) and the procedure code (CPT or HCPCS code) submitted on a claim. In simpler terms, this denial happens when the insurance company determines that the diagnosis does not support the medical procedure or service that was performed.
Let’s understand with a simple example
If a patient is diagnosed with a minor condition, like a cold, but the claim includes a procedure that requires a much more serious diagnosis, such as surgery, the insurer may reject the claim with Denial Code 11. The insurance company is saying that the diagnosis doesn't justify the procedure in question according to their medical policies or guidelines.
Most Known Denial Code 11 Reasons
When a claim is denied with Denial Code 11 this may sound like a simple coding issue; the reasons behind this denial are usually more specific.Lets see some of the most common causes
1- Lack of Specificity in the Diagnosis Code
A frequent mistake occurs when the diagnosis code is too general or lacks the necessary specificity required by the payer. ICD-10 codes have become highly specific, and using an unspecific diagnosis can lead to mismatches with the procedure code. Insurers expect the exact diagnosis to be tied to the service.
Example: A diagnosis of "cough" (ICD-10 code: R05) might not justify a more complex respiratory treatment or procedure, such as bronchoscopy (a diagnostic procedure to examine the airways), which would require a more specific respiratory diagnosis like chronic obstructive pulmonary disease (COPD).
2- Outdated or Incorrect Procedure Code
Sometimes, Denial Code 11 occurs not because of the diagnosis but because the procedure code itself is outdated, incorrect, or not relevant for the diagnosis. This often happens when:
A provider uses a legacy CPT code that may no longer be valid or has been replaced with a new code.
An incorrect procedure modifier is used, creating a mismatch.
Example: A provider submits a claim with an outdated procedure code for surgical biopsy, but the code has been replaced with a more specific version that includes a different level of service. This would result in Denial Code 11.
3- Incorrect Use of Modifiers
Modifiers provide additional context to procedure codes and can influence the insurer’s determination of medical necessity. A missing or incorrect modifier could lead to a denial when there is a need to clarify the relationship between the diagnosis and the procedure.
Example: A claim is submitted for a surgical procedure that requires a bilateral modifier (50) to indicate that the procedure was performed on both sides of the body. If the modifier is left out or incorrectly applied, it could trigger a mismatch with the diagnosis or lead to a denial under Denial Code 11.
4- Medical Necessity Not Supported by Diagnosis
Even when a diagnosis code and procedure code technically match, there may be an issue of medical necessity. Insurers will reject a claim if they determine that the procedure is not warranted based on the diagnosis, even if the codes themselves align.
Example: A diagnosis of "Acute Sinusitis" might be billed with a sinus surgery (functional endoscopic sinus surgery, or FESS). However, unless the sinusitis is recurrent or severe, insurers may consider surgery unnecessary and deny the claim with Denial Code 11.
5- Documentation Lacking Support for the Diagnosis-Procedural Link
Sometimes, the codes themselves may be correct, but insufficient documentation doesn’t show a clear connection between the diagnosis and the procedure. In these cases, the insurer may not accept the claim without more detailed documentation that justifies the medical decision.
Example: A provider submits a claim for knee surgery following a diagnosis of knee pain (ICD-10 code: M25.561). However, the documentation doesn’t include the necessary details, such as diagnostic tests, imaging, or other supporting documentation, showing that surgery was medically necessary. The insurer denies the claim with Denial Code 11.
What to Do If Your Practice Has Encountered a CO 11 Denial Code?
When your practice encounters CO 11, it signals that the diagnosis and procedure codes don’t match according to the insurance company's guidelines. This can be frustrating, but with a structured, step-by-step process, you can quickly resolve the issue and prevent similar denials in the future.
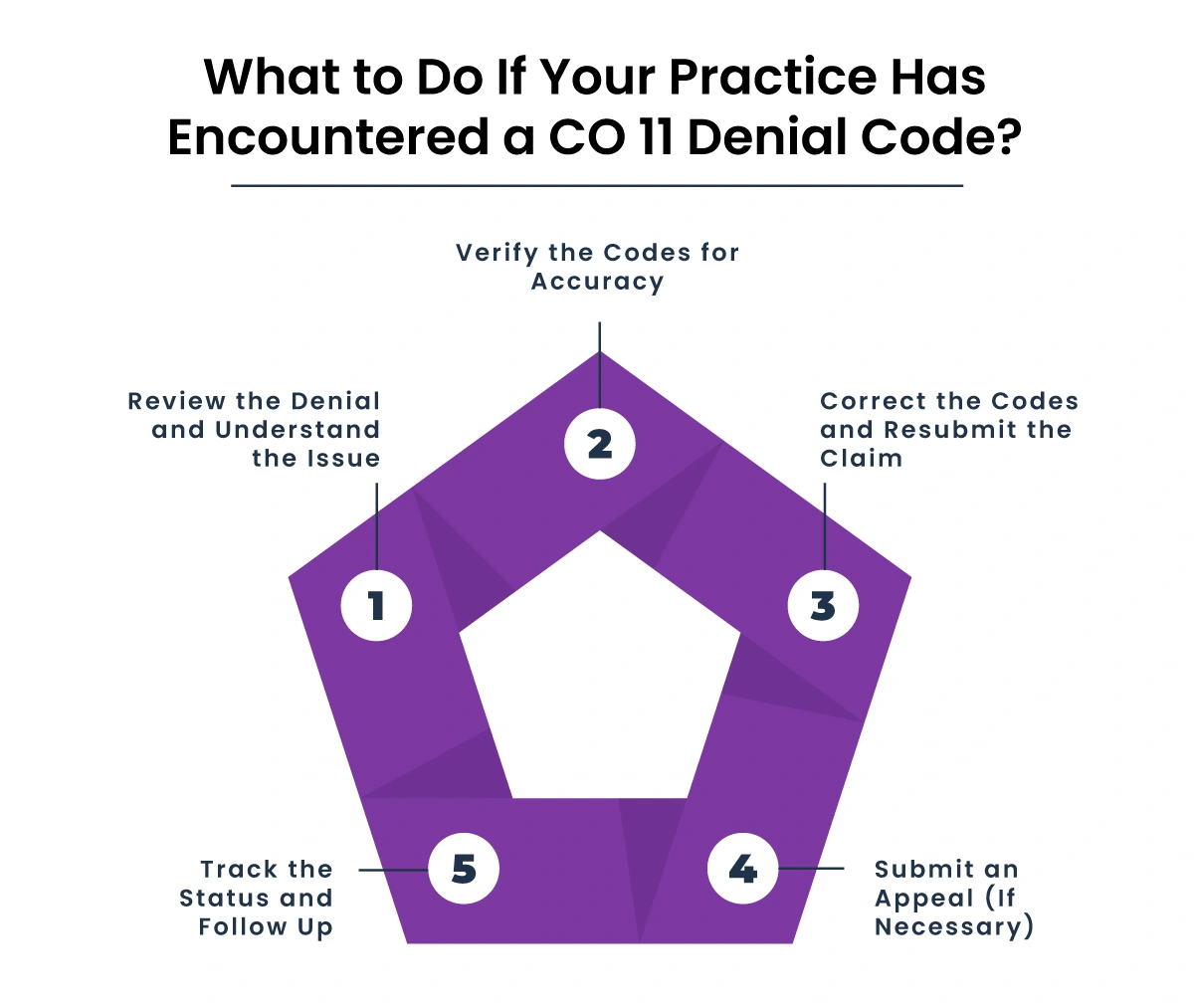
Step 1: Review the Denial and Understand the Issue
The first thing to do when receiving a CO 11 denial is to fully understand the reason behind it. The insurance company will typically provide a brief description of the issue, but it’s essential to dig deeper:
-
Look at the Explanation of Benefits (EOB): Review the denial reason provided by the insurance company. Often, they'll specify which procedure code or diagnosis code is in conflict.
-
Confirm the Exact Mismatch: Compare the diagnosis code (ICD-10) with the procedure code (CPT/HCPCS) to see where the discrepancy lies.
-
Is the diagnosis too general?
-
Does the procedure seem too advanced for the given condition?
-
This step is about clarifying the mismatch and ensuring you understand exactly where the breakdown occurred.
Step 2: Verify the Codes for Accuracy
Once you’ve identified the cause of the denial, the next step is to verify the codes that were submitted.
-
Check Diagnosis Codes: Ensure the diagnosis code is specific enough. Many times, the issue arises from a diagnosis code that is too vague. For example, a code for "abdominal pain" is too broad to justify a complex procedure like laparoscopic surgery. Use the most specific ICD-10 codes possible to ensure the procedure aligns with the diagnosis.
-
Review Procedure Codes: Confirm that the CPT/HCPCS code is appropriate for the condition diagnosed. Sometimes, an outdated or incorrect procedure code is used that doesn't match the clinical service provided. Ensure you are using the most current codes.
-
Check for Modifiers: Review whether the correct modifiers are applied. For instance, certain procedures may require modifiers like -50 for bilateral services or -59 for distinct procedural services. Missing or incorrect modifiers can lead to mismatched claims and denials.
Step 3: Correct the Codes and Resubmit the Claim
If you've identified errors in the diagnosis or procedure codes, you’ll need to correct and resubmit the claim.
-
Correct Diagnosis or Procedure Code: Make the necessary changes to the diagnosis or procedure code to better reflect the clinical scenario. If the diagnosis code was too general, select a more specific one. If the procedure code was outdated or incorrect, ensure it reflects the actual service provided.
-
Include Proper Documentation: If the procedure was indeed medically necessary and supported by the diagnosis, gather supporting documents (e.g., clinical notes, imaging reports, test results) to justify the claim. This is especially important if the procedure seems complex or borderline for the given diagnosis.
-
Double-Check Modifiers: Ensure that modifiers are correctly applied to explain the relationship between the diagnosis and the procedure (if needed).
Step 4: Submit an Appeal (If Necessary)
If, after reviewing and correcting the claim, you still believe the procedure is medically necessary and the codes are correct, you may need to submit an appeal.
-
Prepare Your Appeal: Create a well-documented appeal, providing additional clinical evidence or clarifications that demonstrate the relationship between the diagnosis and the procedure. Attach supporting documents, such as progress notes, diagnostic test results, and any other relevant documentation that supports the medical necessity of the procedure.
-
Follow Insurance Guidelines for Appeals: Every payer has specific guidelines for submitting appeals. Make sure you follow these instructions carefully, including the timeline for submitting appeals (many insurers have strict deadlines).
-
Provide Clear Rationale: In your appeal, explain why the procedure is appropriate for the diagnosis and why the claim should be reconsidered. This might include citing clinical guidelines or providing a detailed justification of the treatment plan.
Step 5: Track the Status and Follow Up
Once you’ve resubmitted the claim or filed an appeal, the next step is to track the status of the claim.
-
Monitor the Claim: Use your practice management software to track the claim's status. Many systems allow you to follow claims through the process and flag them when action is needed.
-
Follow Up with the Payer: If you don’t receive a response within the expected timeframe, don’t hesitate to call the payer’s claims department to check the status and ask for more information.
Be proactive and persistent. Sometimes claims get delayed simply due to processing backlogs, and a follow-up can help move things along.
How To Prevent This CO-11 Denial Code In the Future?
After resolving the immediate issue with the CO 11 denial, it's time to take a step back and consider ways to prevent future denials. These best practices can help avoid a repeat of the same issue:
Ensure your coding and billing staff are properly trained on the importance of matching diagnosis and procedure codes. Continuous education on ICD-10 and CPT updates is essential.
Make sure that your clinical documentation is clear, thorough, and always supports the billed codes. This includes documenting the medical necessity of the procedure and providing detailed notes for any complex treatments or surgeries.
Many practices use code-checking software to verify that the selected diagnosis codes and procedure codes match before claims are submitted. These tools can catch errors before the claims go out the door.
Consider implementing internal audits to pre-emptively catch mismatches in diagnosis and procedure codes before they’re sent to the insurance company.
To take the burden of managing denials off your practice, partnering with an experienced medical billing company like HMS USA LLC can provide substantial benefits. HMS USA LLC specializes in Denial Management Services, focusing on reducing denials and improving cash flow by handling all aspects of claims management, from coding and submission to appeals and follow-up.
ABOUT AUTHOR

Pedro Collins
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.