Every claim denied is a blow to a provider's bottom line. But when it comes to CO 252, the sting is particularly sharp. This seemingly innocuous denial code, signaling a need for "additional information," hides a frustrating reality: even when every box is checked, nearly one in three claims are rejected. The result? A cascade of lost revenue, strained administrative resources, and delayed patient care.
But what if you could crack the CO 252 code? What if you could understand its nuances, anticipate its triggers, and arm yourself with strategies to minimize its impact? In this deep dive, we unravel the mysteries of this pervasive denial, equipping you with the knowledge to fight back and protect your practice's financial health.
What is CO 252 Denial Code?
CO 252, in essence, is a request for more information. It signals that the payer requires additional documentation or clarification to process the claim. In the denial letter it is quoted as
“ An attachment/other document is required to adjudicate this claim/service. At least one remark code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT)”
A large hospital system faced a significant challenge, with approximately 4,223 claims denied due to CO 252. This resulted in a staggering $122,302,768.04 in lost revenue between January and October 2023, highlighting the substantial financial impact of this common denial code.
These staggering losses demand action. If you're struggling to navigate denial CO 252, HMS's U.S.A-based expert billing team is ready to help. Don't let denied claims drain your revenue – request a consultation today.
Factors That Trigger CO-252 Denial Code
The ambiguity of CO 252 stems from its broad applicability. It can be triggered by various factors, including:
-
Missing or incomplete documentation: This could range from patient demographics and insurance information to clinical notes and medical necessity documentation.
-
Coding errors: Incorrect or unspecified procedure codes can lead to CO 252 denials.
-
Prior authorization or referral issues: If services require pre-authorization or a referral, and these are not obtained or documented correctly, CO 252 may be the result.
-
Lack of medical necessity: Payers may request additional documentation to substantiate the medical necessity of the services provided.
How To Manage Denial Code CO-252?
When confronted with the frustrating CO-252 denial, proactive and strategic action is key. Here's a breakdown of how providers can effectively manage this common challenge:
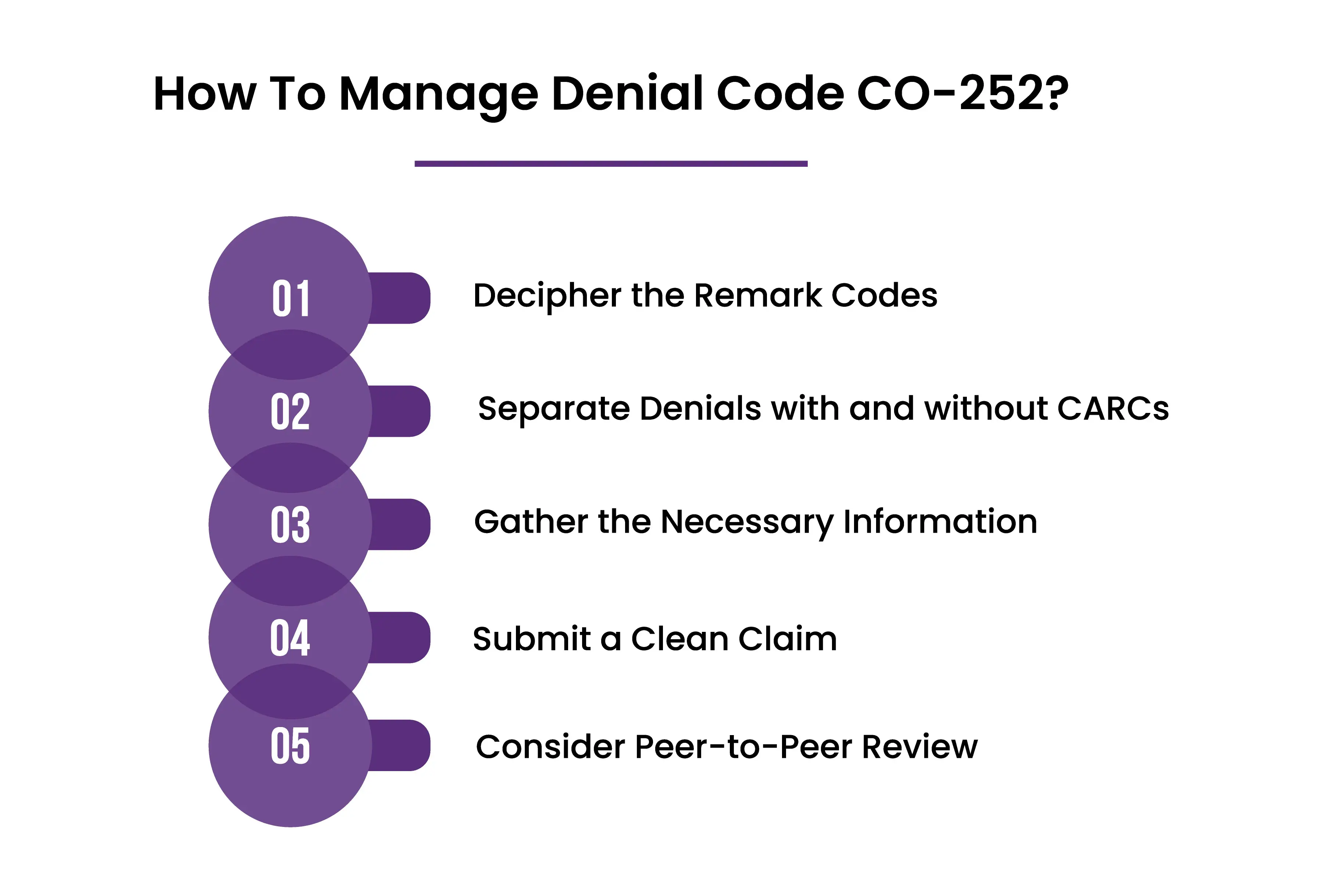
Decipher the Remark Codes: The first step is to carefully review the remittance advice and identify any accompanying remark codes. These codes provide crucial clues about the specific information the payer needs. Think of them as the treasure map guiding you toward a successful appeal.
Separate Denials with and without CARCs: Not all CO-252 denials come with Claim Adjustment Reason Codes (CARCs). If a CARC is present, it indicates that the claim can potentially be corrected and resubmitted. If no CARC is attached, you'll likely need to initiate a more formal appeal process.
Gather the Necessary Information: Once you understand the remark codes, meticulously gather all the requested documentation. This might include patient records, clinical notes, test results, or any other information that supports the medical necessity and appropriateness of the services provided.
Submit a Clean Claim: Ensure that your resubmitted claim is complete, accurate, and free of errors. Double-check all coding, patient demographics, and insurance information. A clean claim significantly increases your chances of a favorable outcome.
Consider Peer-to-Peer Review: If the denial persists despite providing the requested information, a peer-to-peer review may be necessary. This involves a discussion between your physician and a medical reviewer from the payer's organization. It allows for a direct exchange of clinical information and can help clarify any misunderstandings or disagreements about the medical necessity of the services.
What are the Remark Codes that are attached To CO 252?
Some of the most frequent Remark Codes (RARCs) associated with CO 252 denials include:
-
N479: Missing Explanation of Benefits (Coordination of Benefits or Medicare Secondary Payer).
-
N710: Missing notes
-
N712: Missing summary
-
N714: Missing report
-
N716: Missing chart
These remark codes offer valuable clues about the specific missing information the payer requires to process the claim. It is essential to carefully review these codes and provide the necessary documentation to avoid further delays or denials.
Words By Author
CO 252 denials may be a common roadblock in medical billing, but they don't have to be a dead end. By understanding the nuances of this code, deciphering remark codes, and proactively addressing payer requests, providers can significantly improve their claim success rates and safeguard their revenue.
Remember, every denied claim represents an opportunity to learn, adapt, and strengthen your billing processes. Don't let CO 252 stand in the way of providing quality patient care and maintaining a thriving practice. Arm yourself with knowledge, implement effective strategies, and reclaim control over your financial well-being.
ABOUT AUTHOR

Khabib Makhachev
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.