No healthcare provider enjoys seeing a denial code on their claims. It's frustrating, time-consuming, and directly impacts your bottom line. But when that code is CO 96, signaling a non-covered service, a special kind of dread can set in.
Suddenly, it's not just a billing error - it's a potential patient conflict, a challenge to your revenue cycle, and a test of your team's expertise. If you're a healthcare provider, chances are you've encountered the frustrating CO 96 denial code. It signals that the services you provided were deemed "non-covered" by the patient's insurance.
While it might seem like a minor setback, repeated CO 96 denials can significantly impact your practice's financial health. In this survival guide, we will equip you with the knowledge and strategies you need to understand, prevent, and overcome CO-96 denials.
We'll explore the common reasons behind these rejections, share best practices for clean claims submission, and provide practical tips for appealing denied claims successfully.
What is CO 96 Denial Code?
The CO 96 denial code, often accompanied by the phrase "Non-Covered Charge," serves as a signal from insurance payers that a specific service or procedure billed on a claim falls outside the scope of the patient's insurance coverage.
Possible CO 96 Denial Code Reason
Several factors can contribute to a CO-96 denial:
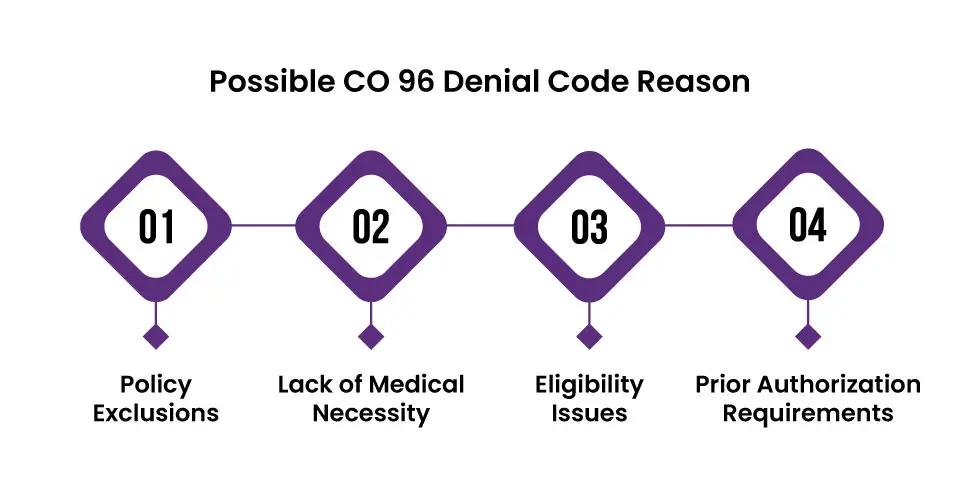
Policy Exclusions:
The patient's insurance plan might specifically exclude the service or procedure rendered. This could be due to the nature of the treatment, the patient's specific plan limitations, or the presence of pre-existing conditions.
Lack of Medical Necessity:
Insurance companies often require that services be deemed "medically necessary" for coverage. If the payer determines the treatment wasn't essential for the patient's condition, a CO 96 denial might result.
Eligibility Issues:
Sometimes, the denial stems from issues with the patient's insurance eligibility. This could include:
-
Inactive Coverage: The patient's insurance might have lapsed or been inactive on the date of service.
-
Incorrect Patient Information: Errors in the patient's demographic or insurance details can lead to eligibility verification failures.
-
Plan Limitations: The patient's plan might have specific restrictions on providers, facilities, or geographic locations.
Prior Authorization Requirements:
Some procedures or medications necessitate prior authorization from the insurance company. If this step is missed, a CO 96 denial is likely.
Denial Code CO-96 Solutions
When you encounter a CO-96 denial code, it's essential to take swift and strategic action to resolve the issue and secure proper reimbursement.
Thoroughly Review the Remittance Advice (RA) or Explanation of Benefits (EOB):
-
Carefully examine the denial reason provided. The RA or EOB should specify why the service was deemed non-covered.
-
Pay close attention to any additional notes or instructions provided by the payer.
Verify Patient Eligibility and Coverage:
-
Double-check the patient's insurance information, including their effective date of coverage, policy limitations, and any exclusions.
-
Contact the insurance company directly to confirm coverage details for the specific service or procedure.
Prior Authorization:
-
If prior authorization was required but not obtained, explore the possibility of a retroactive authorization.
-
If retroactive authorization is not possible, consider appealing the denial with supporting documentation.
Appeal the Denial:
-
If you believe the denial is incorrect or there are extenuating circumstances, initiate the appeals process with the insurance company.
-
Craft a well-structured appeal letter, clearly outlining the reasons for the appeal and providing all relevant supporting documentation.
-
Follow the payer's specific appeal guidelines and deadlines.
Patient Communication:
-
If the denial is upheld, communicate with the patient transparently and compassionately.
-
Explain the reason for the denial and discuss potential options, such as:
-
Billing the patient directly for the non-covered services.
-
Exploring financial assistance programs or payment plans.
-
Recommending alternative treatment options that might be covered.
-
What are remark codes used with CO 96 Denial Code?
CO 96 denials typically do NOT have specific remark codes associated with them. This is because the CO 96 code itself indicates the general reason for the denial, which is a non-covered charge.
However, some payers might include additional information or explanations in the remittance advice or explanation of benefits (RA/EOB) alongside the CO 96 denial. These explanations could provide more context about the specific reason for the non-coverage, such as policy exclusions, lack of medical necessity, or other factors.
How to Prevent CO 96 Denial Code?
Preventing CO 96 denials requires a proactive and multi-faceted approach. Here are some key strategies healthcare providers can implement:
-
Verify the patient's insurance information, including their effective date of coverage, policy type, and any exclusions or limitations
-
Don't just verify eligibility; confirm coverage for the specific services or procedures planned. Contact the insurance company directly if necessary.
-
Familiarize yourself with the payer's prior authorization requirements and identify which services or procedures necessitate it.
-
Initiate the prior authorization process well in advance of the scheduled service.
-
Discuss insurance coverage and potential out-of-pocket costs upfront with patients.
-
Ensure patients understand their financial responsibility for non-covered services.
-
Regularly review claim denials to identify recurring patterns or issues.
-
Maintain open communication with insurance companies to address any questions or concerns promptly.
ABOUT AUTHOR

John Wick
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.
