Imagine this: You've meticulously prepared a claim, sent it off, and eagerly awaited reimbursement. But then, the dreaded denial arrives, stamped with the cryptic "Denial Code CO 97." Frustration sets in. What does it mean? Why did it happen? And, most importantly, how can you fix it?
In this blog post, we'll pull back the curtain on Denial Code CO 97. We'll break down its meaning, explore the common reasons behind it, and equip you with a clear, actionable plan to address it effectively. No more confusion, no more lost revenue.
Denial Code CO 97 Description
Denial Code 97, also referred to as CO 97, signals that the insurance company has already paid for a service or procedure in another payment or allowance. In simpler terms, the payer is saying, "We've already covered this; it's not eligible for separate payment."
This denial can be particularly perplexing because it may appear that a legitimate service was provided and billed correctly. However, the payer is indicating that the cost of this service was bundled or included within another payment, perhaps for a more comprehensive procedure or a global billing period.
Watch Out for The Services That Can Trigger CO 97 Denial Code
While Code 97 denials can seem arbitrary, they often stem from specific billing practices that inadvertently trigger the payer's bundled payment logic. Recognizing these potential pitfalls is the first step towards preventing them. Let's take a closer look at some common services that frequently raise red flags and result in CO 97 denials.
E/M Services during Global Periods:
Evaluation and Management (E/M) services provided within the post-operative period of a surgery are typically bundled into the global surgical package and are not separately billable. This global period can range from 10 days for minor surgeries to 90 days for major surgeries.
Specimen Collection and Handling:
Routine specimen collection (e.g., blood draw) during a patient encounter is often considered an integral part of the visit and not separately billable. Additionally, the transfer and handling of specimens to the lab are usually included in the laboratory service fee.
Certain Surgical Supplies:
Some surgical supplies, like dressings or local anesthesia, may be included in the global surgical package or the facility fee and cannot be billed separately.
Incision and Drainage of a Simple Abscess:
This procedure might be considered part of a more extensive procedure, such as an office visit or another surgical procedure, and therefore not billable separately.
After-Hours Codes for 24-Hour Facilities:
If your practice operates 24 hours a day, billing for after-hours codes might not be allowed as these services are considered part of the regular operations.
Duplicate Billing:
If the same procedure or service is inadvertently billed multiple times for the same date of service, it will likely be denied with CO 97.
Common CARC Codes that Often Accompany a CO 97 Denial
When deciphering a CO 97 denial, it's important to pay attention not just to the denial code itself, but also to the accompanying Claim Adjustment Reason Codes (CARCs). These codes provide valuable clues about the specific rationale behind the payer's decision. Familiarizing yourself with these common CARCs can empower you to pinpoint the issue and take corrective action more efficiently.
-
N120: This code indicates that the denied service or procedure is considered part of the comprehensive E/M service provided on the same day.
-
N372: This code signals that the payer considers the denied service to be inclusive of another, more comprehensive procedure or service that was also billed.
-
N770: This code signifies that the denied service or procedure is bundled or included in the payment for another service, such as a global surgery package or a facility fee.
Your Action Plan for CO 97 Denial Resolution
Receiving a CO 97 denial can be discouraging, but it's not the end of the road. With a strategic approach and a clear understanding of the issue, you can often turn these denials into approvals.
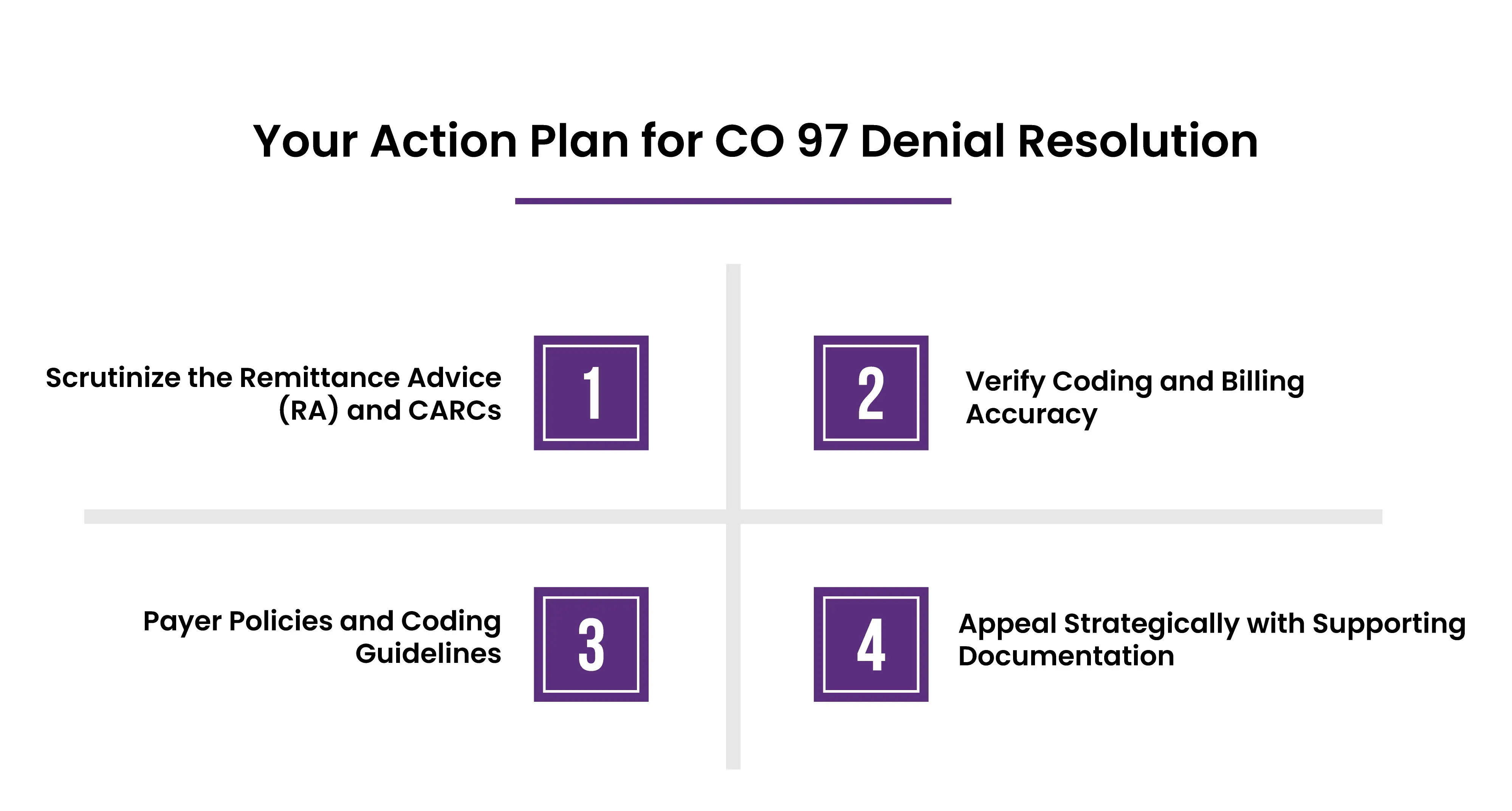
1. Scrutinize the Remittance Advice (RA) and CARCs
The RA is your roadmap. It outlines the specifics of the denial, including the denied procedure code(s), the amount denied, and often, the CARCs explaining why it was denied.
2. Verify Coding and Billing Accuracy
Did you use the most specific CPT code available for the service provided? Less specific codes can sometimes trigger bundling edits. Are modifiers used correctly? Modifiers can clarify the circumstances of a service (e.g., -59 for distinct procedural service). Double-check that all dates match across the claim and medical record.
3. Payer Policies and Coding Guidelines
Each payer has their interpretation of coding guidelines and what constitutes a bundled service. Find and review their specific policies. The NCCI edits are nationally recognized guidelines identifying code pairs that shouldn't be billed together.
Make sure your coding is NCCI-compliant.If the denial is related to a global surgery period, verify the payer's defined timeframe for that specific procedure.
4. Appeal Strategically with Supporting Documentation
State the facts, reference the specific CARCs, and explain why the service should be paid separately. Attach operative notes, progress notes, or any documentation that supports the medical necessity and distinct nature of the service.
Understand the payer's appeals process and deadlines. Some payers have multiple levels of appeal.
How To Prevent CO-97 Denial In Future?
The best way to deal with denials is to avoid them altogether.
-
Each payer has their own nuanced interpretation of bundling and what constitutes a "separate" service. Go beyond general guidelines and meticulously study each payer's policies regarding global periods, inclusive procedures, and common bundled services.
-
Based on your payer mix and specialties, create an internal list of services that historically trigger CO 97 denials. This allows for heightened scrutiny during the billing process.
-
Be cautious when billing for services provided "incident-to" a physician's service. These services may be considered bundled depending on the payer and specific circumstances.
-
Familiarize your team with mutually exclusive code pairs. These codes represent services that are unlikely to be performed together and may trigger a CO-97 denial if billed on the same date of service.
-
When performing multiple procedures or services on the same day, clearly document the medical necessity and distinct nature of each service in the patient's record.
Final Words
While CO 97 denials can be frustrating, they're not insurmountable. By being proactive, you can prevent them and ensure smoother payments. Stay updated on payer policies, improve your billing processes, and use technology wisely. Knowledge is key. Understanding medical billing helps you overcome challenges, get paid what you're owed, and focus on providing great patient care.
ABOUT AUTHOR

John Wick
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.