Medical credentialing can be a daunting task, especially for small and solo practices with limited resources. From complex requirements to time-consuming processes, it's easy to feel overwhelmed.
However, the importance of effective medical credentialing cannot be overstated. It's crucial for patient safety, revenue generation, and practice credibility.
In this blog, we'll explore the challenges faced by small and solo practices in medical credentialing, as well as how medical credentialing serves as a solution to overcome them.
So, let's dive in and find out how to make the process more manageable and beneficial for your practice!
What Is Medical Credentialing and It’s Process?
Medical credentialing is the process of verifying a healthcare provider's qualifications, experience, and background to ensure that they meet the standards and requirements of healthcare organizations, insurance companies, and regulatory bodies.
This process is necessary for healthcare providers to become eligible for reimbursement from insurance companies, gain hospital privileges, and maintain professional credibility.
Steps Involved in Medical Credentialing Process
The medical credentialing process typically involves several steps which are:
- Verification of provider's qualifications, experience, and background.
- Gathering relevant documentation from educational institutions, licensing boards, and previous employers.
- Conducting background checks, including malpractice history and criminal record.
- Submission of the provider's application for credentialing to the credentialing organization.
- Review of the provider's application by a credentialing committee to determine eligibility for credentialing privileges.
- Decisions made by the credentialing committee based on the provider's qualifications and standards.
- Notification of the provider of the decision on their credentialing application.
- Ongoing monitoring and re-verification of the provider's credentials to maintain credentialing privileges.
How Much Time Is Required to Get Credentialed for Small Practices?
The provider enrollment processing time for small practices can vary depending on several factors, including the complexity of the credentialing requirements, the completeness of the application, the responsiveness of the credentialing organization, and the workload of the credentialing committee.
In general, the credentialing process can take several weeks to several months to complete. For small practices, the time required for credentialing may be longer due to limited resources, lack of expertise, and competing priorities.
It's important to note that the credentialing process is a complex and time-consuming process that requires significant administrative time and resources. Small practices should utilize best credentialing practices by planning ahead and allocate enough time and resources to complete the credentialing process effectively.
Challenges Faced by Small and Solo Practices in Medical Credentialing
Small and solo medical practices face a number of challenges when it comes to medical credentialing. Here are some of the most common ones:

Limited Resources
Small and solo practices often face resource constraints, such as limited staff and financial resources, which can make it challenging to allocate time and resources for the credentialing process.
This can result in delays in completing the application, missing deadlines, and errors in documentation, which can lead to denials or delays in the credentialing process.
Complex Credentialing Requirements
The credentialing requirements can be complex and vary depending on the credentialing organization, making it difficult for small and solo practices to stay up-to-date with the constantly changing regulations.
Credentialing requirements may include verification of education, training, licensure, work history, malpractice history, and criminal record, among other things.
The complexity of these requirements can be overwhelming for small and solo practices, especially if they do not have dedicated staff or expertise in credentialing.
Time-Consuming Process
The credentialing process can be lengthy and time-consuming, requiring significant administrative time and resources. Small and solo practices may struggle to manage the time required for credentialing, as staff may need to focus on other tasks such as patient care, billing, and administrative tasks.
This can result in delays in completing the credentialing application, leading to lost revenue and other negative impacts on the practice.
Credentialing Discrepancies
Discrepancies or errors in the credentialing application can lead to delays in the credentialing process, resulting in lost revenue and other negative impacts on the practice.
Small and solo practices may not have the dedicated staff or expertise in credentialing to ensure that the application is accurate and complete, which can result in delays or denials.
Lack of Experience
Small and solo practices may lack the expertise and knowledge to navigate the credentialing process effectively. This can result in mistakes and delays in completing the credentialing application, leading to negative impacts on the practice's revenue and reputation.
Without the necessary expertise and knowledge, small and solo practices may struggle to understand the requirements and nuances of the credentialing process, resulting in incomplete or inaccurate applications.
Solutions to Overcome Challenges Faced in Medical Credentialing
Small and solo practices can breathe a life if they follow the set of solutions to overcome the challenges and hurdles they face in enrollment and credentialing.
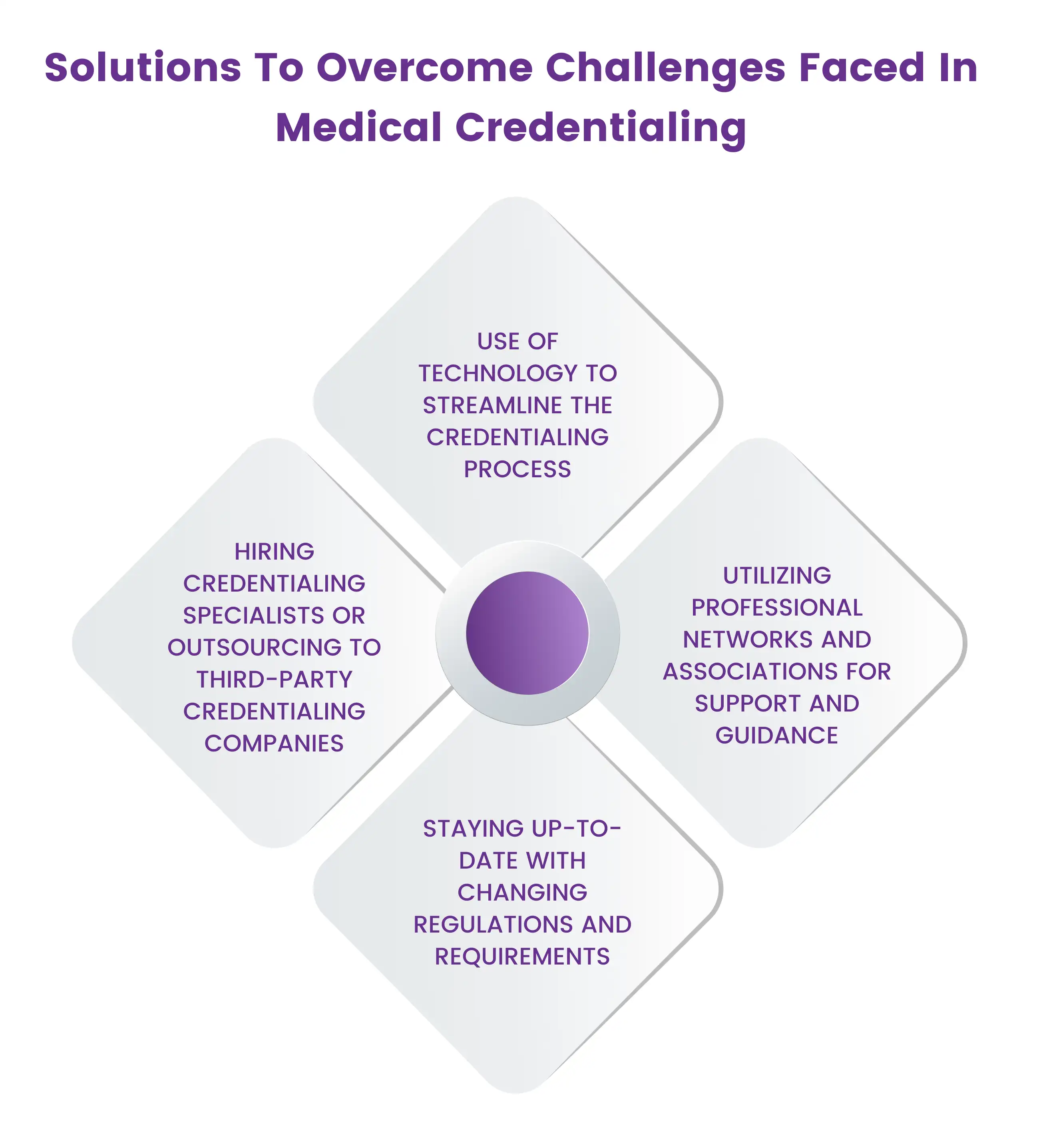
Use of technology to streamline the credentialing process
Small and solo practices can use credentialing software to streamline the credentialing process and automate administrative tasks such as data entry, document management, and application submission. This can help to reduce errors and save time and resources.
This can be achieved by utilizing medical credentialing from a trusted provider as they can help to a smooth credentialing and enrollment process as they have access to the latest technologies and solutions.
Hiring credentialing specialists or outsourcing to third-party credentialing companies
Small and solo practices can hire a credentialing specialist or outsource the credentialing process to a third-party credentialing company. These specialists or companies have the expertise and knowledge to manage the credentialing process effectively, ensuring accuracy, completeness, and timeliness.
Seeking help from a professional provider can be beneficial for the solo and small practices as they will help them to get recognized and will help them to get the accurate provider reimbursement for the services they have rendered.
Ready to Get Credentialed? Get In Touch now
(212) 363-0114
Staying up-to-date with changing regulations and requirements
Small and solo practices can stay up-to-date with changing regulations and requirements by attending conferences, webinars, and training programs. This can help them to understand the latest credentialing requirements and stay compliant.
Utilizing professional networks and associations for support and guidance
Small and solo practices can utilize professional networks and associations for support and guidance. These networks and associations can provide resources, advice, and support to help small practices navigate the credentialing process more effectively.
Overall, these solutions can help small and solo practices to overcome the challenges of medical credentialing, ensuring that the process is completed efficiently and effectively, leading to improved patient safety, increased revenue, and enhanced practice reputation and credibility.
Final Words
In conclusion, medical credentialing can be a daunting task for small and solo practices, but it's essential for maintaining professional credibility and generating revenue. The challenges faced by these practices can be overcome by utilizing technology, hiring credentialing specialists or outsourcing to third-party Company.
If you own or run a solo or small practice and are continuously struggling with medical credentialing, consider seeking assistance from a trusted provider like HMS USA LLC. With our expertise and advanced technology solutions, we can help streamline the credentialing process and ensure accuracy and completeness in your applications. Contact us today@ (212) 363-0114 or you can mail us out at Info@hcmsus.com.
ABOUT AUTHOR

John Bradshaw
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.