Wound care is a crucial aspect of healthcare, as it involves treating and managing various types of wounds, such as cuts, burns, and pressure ulcers. As a healthcare provider, it is essential for you to understand the billing and coding guidelines for wound care in order to ensure timely and accurate reimbursement.
In this blog guide, we are going to discuss the important guidelines for wound care billing and coding that can help you capture higher reimbursements. So all you need to do is continue reading.
Types Of Wounds
Before stepping into one of the most crucial aspects of wound care billing and coding, let's look into the different types of wounds. According to the Centers for Medicare and Medicaid Services (CMS), there are four types of wounds that fall under wound care billing:
-
Acute Wounds
-
Chronic Wounds
-
Open Wounds
-
Closed Wounds
For each type of wound, specific billing codes are used to capture the services provided and determine reimbursement accurately.
CMS Billing Guidelines for Wound care
Wound care procedures are normally performed to help speed up the healing process and prevent infection. When billing for wound care services, it is important to follow CMS guidelines to ensure proper reimbursement.
Purpose of Active Wound Care Procedures
Active wound care procedures are performed to promote healing by removing devitalized or necrotic tissue. Providers bill for these services when they thoroughly need to clean a wound before applying dressing. Debridement is crucial, involving removing foreign objects and bad tissue until only healthy tissue remains.
Often Used CPT Codes For Wound Care Services
You need to use CPT 97597 & CPT 97598 for specific wound care services.
-
CPT 97597- Debridement (removal of damaged tissue), open wound, including topical application(s), wound assessment, use of a whirlpool, first 20 sq cm or less.
-
CPT 97598- Each additional 20 square centimeters of debridement
-
CPT 97602- Application of dressing(s) to open wounds with topical medication(s) (e.g., wet to dry dressing, enzymatic debridement), including negative pressure wound therapy pump management, per session
-
CPT 97605- Debridement of skin or subcutaneous tissue by mechanical methods (e.g., curettage, dermabrasion), per session
-
CPT 97606- Instillation of medication(s) into open wound(s) through a peripherally inserted catheter (PICC) or central venous catheter (CVC), per session
11000-11012: These codes cover the debridement of various skin and subcutaneous tissues. The specific code used depends on the depth and size of the wound.
11042-11047: These codes cover sharp debridement of wounds, which is a more aggressive type of debridement that removes deeper tissue.
Debridement Criteria:
To bill using CPT codes 97597 and 97598, you need to see bad, dead tissue (necrotic tissue). Simply removing fluids or secretions doesn't count; we must remove bad tissue.
When Not to Use Other Codes:
You shouldn't use these codes for some other wound treatments, like cleaning debris, treating corns, draining abscesses, nail care, treating acne, removing warts, or burn care. Use the right codes for these.
Billing Criteria for Hydrotherapy (Whirlpool):
If you are billing for hydrotherapy along with CPT codes 97597 or 97598, we must explain why it was needed to remove bad tissue. We should also show that a physical therapist was needed for the treatment. You can't bill separately for whirlpool treatments (CPT code 97022) if it's for the same body part as wound care with CPT codes 97597-97598.
Local Anesthesia:
The cost of numbing the area with local anesthesia is already included in the debridement payment and shouldn't be billed separately.
Home Health and Part B:
Home health agencies or Part B may cover billing for "sometimes" therapy codes (CPT 97597 and 97598), depending on who's providing the service.
Coding Guidelines for Wound Debridement
To specify the type of debridement performed, you must use the cpt code from (11042-11047) depending upon the depth of tissue removed and the surface are of wound.
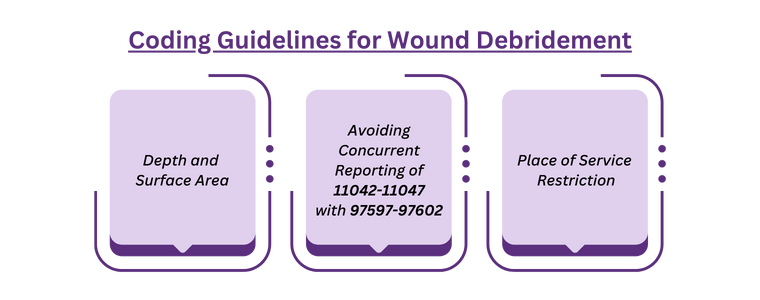
Depth and Surface Area:
Single Wound: If debridement is done on a single wound, the coding should reflect the deepest level of tissue removed.
Multiple Wounds: When multiple wounds are treated, you should sum the surface areas of wounds at the same depth. However, you must not combine the sums of wounds at different depths.
Avoiding Concurrent Reporting of 11042-11047 with 97597-97602:
Do not use codes 11042-11047 in conjunction with 97597-97602 for the same wound. This is likely to prevent billing for overlapping or duplicated services.
Place of Service Restriction
When the service is provided in specific settings - inpatient hospital, outpatient hospital, or ambulatory surgical center (ASC). Use CPT 11043, 11046, 11044, 11047. These are specifically used for deep debridement procedures that reach down to the muscle and bone.
Modifiers Commonly Used in Wound Care Billing
In addition to the CPT codes you mentioned, several modifiers are frequently used in wound care billing to provide additional information about the services rendered. Here are some of the most common ones:
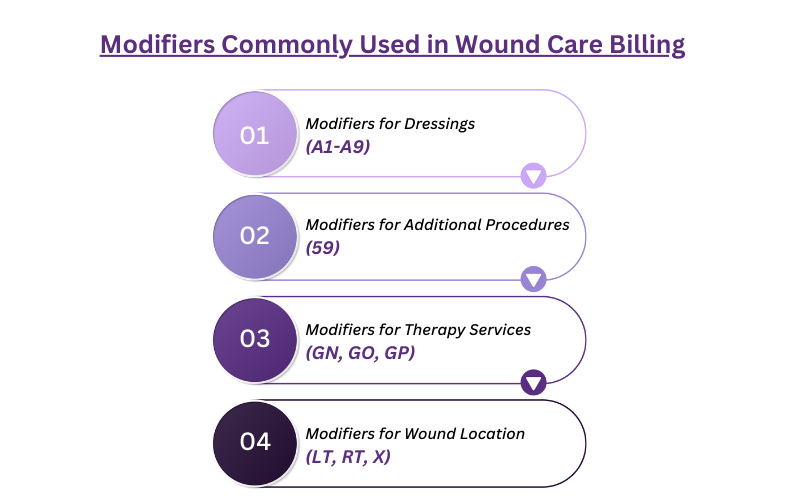
Modifiers for Dressings (A1-A9):
These modifiers indicate the number of wounds a dressing is applied to (e.g., A1 for primary dressing on one wound, A5 for secondary dressing on five wounds).
Modifiers for Additional Procedures (59):
This modifier signifies a distinct and separate service performed during the same encounter as the primary procedure (e.g., debridement of multiple wounds).
Modifiers for Therapy Services (GN, GO, GP):
These modifiers denote the type of therapy performed by a therapist for wound care (e.g., GN for new patient evaluation, GO for individual therapy, GP for group therapy).
Modifiers for Wound Location (LT, RT, X):
These modifiers specify the laterality of the wound (e.g., LT for left leg, RT for right arm, X for bilateral).
Denials Commonly Encountered in Wound Care Billing
Wound care billing can be complex and prone to denials due to various factors. Here are some of the most common denial reasons specific to wound care:
Medical Necessity:
Lack of documentation: Insufficient documentation supporting the medical necessity of the service is a major cause of denials. This includes:
-
Inadequate details about the wound size, depth, location, and stage.
-
Missing information about the type and severity of infection, if present.
-
Lack of justification for specific treatments or procedures.
Non-covered services: Billing for services not covered by the patient's insurance plan, such as experimental treatments or cosmetic procedures.
Frequency of debridement: Debridement exceeding the medically necessary frequency based on wound healing progress.
Coding Errors
Incorrect CPT codes: Using the wrong code for the service provided can lead to automatic denials.
Missing or inaccurate modifiers: Not using appropriate modifiers to explain specific details of the service can result in denials.
Bundled services: Billing for services already included in another code is considered unbundling and can be denied.
Administrative Errors
Missing or inaccurate patient information: Incorrect demographic details or insurance information can lead to claim denials.
Late claim submission: Exceeding the deadline for submitting claims can result in automatic denial.
Prior authorization: Failure to obtain prior authorization for required procedures can lead to denials.
Additional Denial Reasons
Exceeding frequency or duration limits: Billing for more services than allowed within a specific timeframe.
Not meeting quality-of-care standards: Denials based on concerns about the quality of care provided.
Duplicate billing: Billing for the same service multiple times.
Tips to Reduce Denials
-
Document all aspects of the wound care encounter in detail.
-
Ensure you use the latest and accurate CPT codes and modifiers.
-
Confirm the services are covered by the patient's insurance plan before providing them.
-
Follow the insurance company's deadlines for claim submission.
-
Consider seeking assistance from a professional to ensure accurate coding and claim submission.
Words By Author
Wound care billing can be challenging due to the various factors that can lead to claim denials. It is essential to understand the coding guidelines and use appropriate modifiers to support the medical necessity of the services provided. By following these tips and being vigilant in documentation, you can increase the chances of successful reimbursement for wound care services.
So, it is crucial to stay updated if you are struggling with the intricacies of wound care billing, consider the benefits of outsourcing to specialists like HMS Wound Care Billing services. By leveraging their expertise, you can streamline your billing processes, reduce denials, and ensure that your focus remains on delivering quality patient care.
ABOUT AUTHOR

Doron
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.
