Effective billing and coding for orthodontic services is essential for accurate claims submission and consistent reimbursement. Given the complex nature of orthodontic procedures, correct coding and billing practices are vital to avoid claim denials and ensure timely payments.
This guide is designed to equip dental professionals with reliable, step-by-step billing and coding instructions for orthodontic services. By implementing these guidelines, practices can improve accuracy, support compliance, and strengthen their overall financial management.
Start With Determining Eligibility
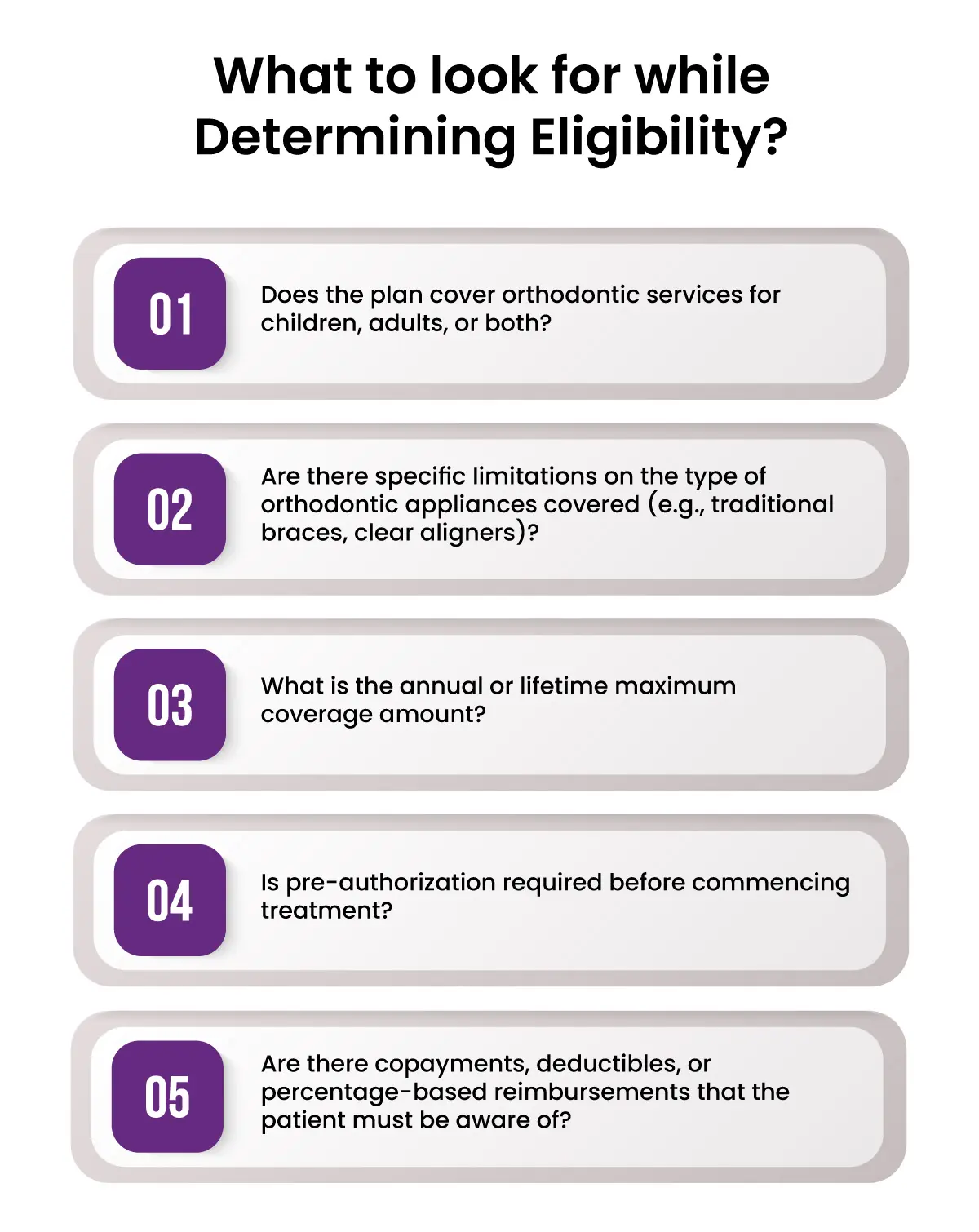
Before initiating any orthodontic treatment, determining the patient’s insurance eligibility is a crucial first step. Proper verification not only sets clear expectations for the patient regarding their financial responsibility but also minimizes potential disruptions in claim processing down the line. Here's a comprehensive look at how to approach this phase effectively:
Ensuring that the patient’s orthodontic coverage is active and aligns with the proposed treatment plan is essential. Contact the patient’s insurance provider directly to verify coverage details, paying close attention to any specific terms or conditions that may impact the treatment's reimbursement.
This verification should include confirming plan activation, waiting periods, maximum lifetime benefits, and any exclusions related to orthodontic care. Establishing clear communication with the payer allows the practice to avoid misunderstandings and helps prevent denied or delayed claims.
Since orthodontic benefits can vary widely between different insurance plans, using a standardized checklist can streamline the process of gathering necessary information. This checklist should include key questions such as:
-
Does the plan cover orthodontic services for children, adults, or both?
-
Are there specific limitations on the type of orthodontic appliances covered (e.g., traditional braces, clear aligners)?
-
What is the annual or lifetime maximum coverage amount?
-
Is pre-authorization required before commencing treatment?
-
Are there copayments, deductibles, or percentage-based reimbursements that the patient must be aware of?
By collecting these details in a systematic way, the practice can set clear expectations for both the patient and the practice’s billing team, ensuring smoother claim submissions.
Understanding dependent coverage is another critical factor in verifying eligibility. Many insurance plans provide orthodontic benefits specifically for dependents, which often include high school and college-aged individuals.
However, a smaller number of plans extend similar coverage to adult patients. When verifying eligibility, it is important to confirm whether dependent coverage applies and identify any age limitations that could impact treatment timing.
Ensuring that this information is well-documented in the patient’s record helps create transparency and avoids future disputes.
Filing The Claim With ADA Dental Claim Form
When filing an orthodontic claim, utilizing the ADA Dental Claim Form correctly is essential to avoid delays or denials. The 2019 ADA Dental Claim Form, which supports CDT-2020 codes, is the standard for submitting dental claims, including orthodontic procedures.
Attention to accuracy and completeness will ensure a smoother claims process and enhance the likelihood of timely reimbursements. Below is a step-by-step guide to completing the key sections of the form:
Current Form Usage: Ensure that you are using the 2019 ADA Dental Claim Form, as it aligns with the most recent coding standards and accommodates CDT-2020 codes.
Accuracy and Completeness: To prevent delays or denials, it is crucial to fill out all required sections accurately. Double-check each entry for consistency and correctness to avoid resubmissions, which can extend payment timelines.
Key Sections to Complete:
-
Patient Information (Sections 1-23):
Enter the patient’s personal details, including full name, address, date of birth, and insurance ID number. Ensure that any subscriber information, if different from the patient, is accurately reflected.
2. Insurance Policy Information:
Include subscriber details if the insurance policyholder differs from the patient. This ensures that the payer can verify the correct relationship and eligibility.
3. Billing Dentist or Dental Entity (Sections 48-52):
Provide the full name, address, Tax ID number, and National Provider Identifier (NPI) of the dentist or dental entity responsible for billing. Accurate provider details are essential for claims processing and compliance.
4.Ancillary Claim/Treatment Information:
Box 40 (“Is Treatment for Orthodontics?”): Mark “Yes” for all orthodontic claims.
Box 41 (“Date Appliance Placed”): Indicate the exact date the appliances were delivered to the patient, as this is critical for orthodontic claim documentation.
Box 42 (“Months of Treatment”): Specify the total estimated number of active treatment months.
Box 39 (“Radiographs or Models Enclosed”): Usually, mark “No” unless specifically requested by the insurance payer.
5. Record of Services Provided:
Procedure Date (Column 24): Document the date on which each procedure was completed.
Area of Oral Cavity (Column 25): Use appropriate codes if relevant; for orthodontic treatments, this is often coded as “00” for the entire oral cavity or “01” for the maxillary arch.
Tooth Number(s) or Letter(s) (Columns 26 and 27): Typically not required for orthodontic claims, but confirm based on payer-specific rules.
Procedure Code (Column 29): Enter the correct CDT code for each service rendered.
Description (Column 30): Include a brief description of the procedure performed for clarity.
Fee (Column 31): List the fee charged for each service to maintain transparency in billing.
When completing the ADA Dental Claim Form, clearly indicating the total case fee for the orthodontic treatment plan is crucial. The total case fee represents the complete cost of treatment, covering all related services and procedures over the treatment period.
This fee should encompass diagnostic evaluations, appliance fittings, periodic adjustments, and any follow-up visits included within the agreed plan.
For many orthodontic cases, it is common for patients to make an initial down payment before treatment begins. This payment can influence the way the insurance payer views the claim, as it indicates a commitment to cover part of the cost upfront.
When documenting the down payment, specify the amount paid by the patient, the date of payment, and any associated receipt or transaction reference number. This inclusion helps demonstrate that the financial arrangements between the practice and the patient are established and documented, aligning with many payers' requirements for comprehensive claim submissions.
Case classification indicates whether the orthodontic treatment is limited, comprehensive, or another specified category. Limited treatment often addresses a specific part of the dentition or a specific condition, whereas comprehensive treatment involves a full, systematic approach to correcting dental alignment and bite issues.
It is also important to note whether the treatment is being conducted for an adolescent or adult patient, as coverage often differs based on the patient’s age. Classifying the case clearly helps ensure that payers can appropriately match the treatment to their policy guidelines, affecting approval and reimbursement decisions.
The case diagnosis section should include detailed information about the orthodontic condition being treated. This typically involves identifying the malocclusion class—such as Angle Class I (neutrocclusion), Class II (distocclusion), or Class III (mesiocclusion). Each class represents a specific type of dental alignment issue, which helps insurers understand the complexity and necessity of the treatment plan.
Supporting Documentation
Supporting documentation is often essential to back up the details provided on the claim form. Examples of such documentation include:
-
Detailed Treatment Plans: These outline the objectives, phases of treatment, and expected outcomes, giving payers a comprehensive view of what the treatment entails.
-
Narratives: A concise explanation or narrative may be necessary to clarify unique aspects of the treatment plan or justify specific procedural codes used.
-
Radiographs and Clinical Images: While Box 39 generally marks whether radiographs or models are enclosed, providing them may be required if specifically requested by the payer to support the diagnosis and treatment plan.
-
Progress Notes: Regular updates on the patient’s treatment progression, if requested, can validate the necessity and timeline of the ongoing care.
Billing & Coding for Orthodontic
I. Pre-Orthodontic Treatment Visit (D8660)
The pre-orthodontic treatment visit serves as an essential first step in the orthodontic treatment journey, focusing on initial evaluations and monitoring growth and development before active treatment begins. For general practices, this visit may include assessing adult candidates for Invisalign® during routine check-ups.
Billing Practices For Pre-Orthodontic Treatment Visit
Typically, no fee is charged for this visit as it is often provided as a complimentary service. However, some practices may choose to bill for a treatment presentation using code D9450. This code represents the detailed and extensive planning involved in presenting the case to the patient, though it is common for no fee to be associated with it.
Coding for Pre-Treatment Visits
-
D8660: This code is used for pre-orthodontic treatment evaluations to monitor growth and development.
-
D9450: May be used for case presentation involving comprehensive treatment planning, if applicable.
Claim Submission Details
If a practice chooses to bill for this visit, D8660 should be entered in the "Record of Services Provided" section, including the date and associated fee. Additionally, Box 40, which asks, "Is Treatment for Orthodontics?" must be marked as "Yes" to indicate that the visit pertains to orthodontic treatment.
II. Records Visit
The records visit is vital for gathering the diagnostic information needed to create a treatment plan. During this visit, photographs, diagnostic casts, and radiographic images are collected. For Invisalign® patients, impressions or digital scans (such as iTero® scans) may be sent to Align Technology for the creation of a ClinCheck® treatment plan.
Components and Corresponding Codes
Photographic images obtained for diagnostic purposes are coded as D0350. Diagnostic casts, which may be impressions or digital scans, are coded as D0470. These casts help create models for assessment and treatment planning. A D0340 code is used for a 2D cephalometric radiographic image, essential for evaluating skeletal relationships, though it may not be required for every patient.
Advantages of Filing Records Separately
Submitting records separately allows dental practices to verify how the insurance provider handles orthodontic claims before active treatment begins. This approach can accelerate payment for the records portion and act as an early indicator of any potential issues with coverage for the entire case.
Billing Practices for Records Visit
Some practices choose to bill separately for records, which may increase potential reimbursement opportunities. Alternatively, others include records within a global fee, though billing records separately can provide clearer benefits and quicker payments.
Claim Submission Details
Each procedure, such as D0350, D0470, or D0340, should be entered in the "Record of Services Provided" section with the relevant date and fee. Box 40 should be checked "Yes" to confirm that the procedures pertain to orthodontic treatment. Radiographs or models should only be sent if specifically requested by the payer.
III. Treatment Start Visit (Active Appliance Placement)
The treatment start visit marks the beginning of active orthodontic treatment. This is when aligners or other orthodontic appliances are delivered to the patient, indicating the start of the corrective phase.
Case Classification Codes
Orthodontic treatment can be classified as either limited or comprehensive. D8030 and D8040 are used for limited orthodontic treatment of the adolescent and adult dentition, respectively. Comprehensive treatment, coded as D8080 for adolescents and D8090 for adults, involves full treatment of the dentition and correction of malocclusions.
Definitions of Dentition
Adolescent dentition refers to patients with permanent teeth who are still in their growth phase, typically under the age of 18. Adult dentition applies to those whose growth has been completed, generally aged 18 and over.
Claim Submission Details
To properly document this visit, enter the appropriate code (e.g., D8080) in the "Record of Services Provided" section, along with the date and fee. Include detailed notes, such as the total case fee, any down payment made by the patient, and monthly payment terms. Additionally, specify the case classification (limited or comprehensive) and diagnosis type (e.g., Angle Class II malocclusion). Ensure Box 40 is marked "Yes," Box 41 contains the "Date Appliance Placed," and Box 42 reflects the "Months of Treatment."
IV. Periodic Orthodontic Treatment Visit (D8670)
Periodic orthodontic visits during active treatment must be reported to track the progress and may be required by some payers for ongoing reimbursement.
Purpose of Periodic Visits
These visits involve routine checks to monitor the progress of the orthodontic treatment and make necessary adjustments to ensure the treatment stays on track. This is crucial for maintaining effective treatment outcomes and aligning with insurance requirements.
Coding for Periodic Visits
The code D8670 is used to represent a periodic orthodontic treatment visit. The fee reported for these visits typically reflects the total case fee, unless otherwise directed by the insurance provider.
Claim Submission Details
D8670 should be entered in the "Record of Services Provided" section with the date and associated fee. Include the original "Date Appliance Placed" in Box 41 and indicate "Months of Treatment" in Box 42. Confirm that Box 40 is checked "Yes" to indicate orthodontic treatment.
V. Orthodontic Retention (D8680)
The orthodontic retention phase follows the completion of active treatment and focuses on maintaining the results achieved.
Coding for Retention Phase
The code D8680 is used for orthodontic retention. This is usually included in the global case fee, meaning most payers may not be able to provide additional reimbursement.
Coverage Considerations
Orthodontic retention is often part of the global fee associated with the treatment, so separate billing may be denied or marked as non-billable. However, if separate billing is attempted, practices should be prepared for it to be disallowed by the payer.
Claim Submission Details
Enter D8680 in the "Record of Services Provided" section, along with the date and fee, if billing separately. Include the "Date Appliance Placed" in Box 41 and "Months of Treatment" in Box 42. Ensure Box 40 is checked "Yes," and specify the area of the oral cavity involved in Box 25.
Replacement of Retainers
Replacement of retainers, coded as D8703 for the maxillary arch and D8704 for the mandibular arch, is typically considered the patient’s responsibility as it may fall outside the lifetime benefit coverage.
Typical ADA Codes for Limited and Comprehensive Invisalign® Cases
Understanding the appropriate ADA codes for various types of Invisalign® cases is essential for accurate billing and claim submission. These codes help differentiate between the scope and complexity of treatment, ensuring that the correct procedures are documented and reimbursed appropriately. Below are the typical ADA codes used for limited and comprehensive orthodontic treatments.
Limited Orthodontic Treatment Codes
Limited orthodontic treatment focuses on achieving a specific, defined objective without addressing the entire dentition. The following codes are used to document such cases:
-
D0810 – Limited orthodontic treatment of the primary dentition
Used when treatment is focused on primary (baby) teeth.
-
D8030 – Limited orthodontic treatment of the adolescent dentition
Applies when treatment targets adolescent patients who have some or all permanent teeth but whose growth is still ongoing.
-
D8040 – Limited orthodontic treatment of the adult dentition
Used for limited orthodontic cases involving adult patients with fully developed permanent dentition.
Comprehensive Orthodontic Treatment Codes
Comprehensive orthodontic treatment involves full correction of malocclusion and alignment issues across the entire dentition. This type of treatment is typically more extensive and may span a longer duration. The following codes represent comprehensive cases:
-
D8070 – Comprehensive orthodontic treatment of the transitional dentition
Used for cases involving patients with a mix of primary and permanent teeth, often during the transition to full permanent dentition.
-
D8090 – Comprehensive orthodontic treatment of the adult dentition
Applies to adult patients who require full treatment for complete correction of alignment and bite issues.
Final words
Lastly, it goes without saying that by adhering to well-structured protocols—ranging from verifying insurance eligibility and correctly completing the ADA Dental Claim Form to understanding the ADA codes for limited and comprehensive Invisalign® cases—dental practices can significantly reduce claim denials and optimize their revenue cycle. The goal is to streamline operations so that providers can focus on delivering exceptional patient care without the stress of billing issues.
However, managing these processes can be overwhelming without expert assistance. HMS USA LLC offers dedicated Dental billing services designed to take the complexity out of coding and claims management. With their specialized knowledge and experience, HMS USA LLC helps dental practices enhance their billing efficiency, reduce administrative burdens, and secure the revenue they deserve.
ABOUT AUTHOR

Pedro Collins
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.