As a healthcare provider, you know the value of well-child exams in supporting a child’s health and development. However, ensuring these visits are coded and billed accurately is often a challenge. With evolving payer guidelines and the need to capture additional services, such as immunizations or screenings, even experienced professionals can face obstacles in getting claims approved. This blog offers a straightforward approach to help you master the essentials of well-child exam coding.
Primary CPT Codes for Well-Child Exam
The American Medical Association (AMA) has outlined specific CPT codes to document these visits, tailored to the patient’s age and whether they are a new or established patient. Understanding these distinctions is crucial for accurate billing and reimbursement.
Well Child Exam For New Patient
For new patients, who are visiting the practice for the first time, CPT codes 99381–99385 are used. These codes are age-specific:
CPT Code 99381: Well Child Exam for Infant (younger than 1 year)
This code is used for infants during their first year of life, a period of rapid growth and development. The well-child exam for this age group typically includes:
-
A comprehensive review of the child’s birth history and family medical history.
-
Detailed measurements, such as weight, length, and head circumference, to assess growth patterns.
-
Physical examinations focusing on identifying congenital conditions, ensuring normal reflexes, and evaluating sensory and motor development.
CPT Code 99382: Well Child Exam for Early Childhood (ages 1–4 years)
During early childhood, the focus shifts to monitoring growth milestones and behavioral development. This code applies to visits for toddlers and preschoolers, encompassing:
-
Assessment of motor skills, language development, and social interactions to ensure appropriate developmental progress.
-
Growth tracking through weight, height, and body mass index (BMI) measurements.
-
Physical examination, including checks for vision and hearing abnormalities.
-
Immunization updates as recommended by the ACIP (Advisory Committee on Immunization Practices) schedule.
-
Parental counseling on nutrition, safety measures (e.g., car seats, childproofing), and behavioral issues such as sleep or temper tantrums.
CPT Code 99383: Well Child Exam for Late Childhood (ages 5–11 years)
This code covers school-aged children, emphasizing academic readiness and social integration. Key components of this well-child exam include:
-
Evaluation of cognitive development and school performance, addressing any concerns such as learning disabilities or ADHD.
-
Routine physical checks, including weight, height, and screening for scoliosis or other musculoskeletal issues.
-
Continued monitoring of immunizations, including booster doses of previously administered vaccines.
-
Discussion with parents and the child about healthy eating habits, physical activity, and maintaining good hygiene.
-
Screening for common conditions in this age group, such as anemia, asthma, or allergies.
CPT Code 99384: Well Child Exam for Adolescents (ages 12–17 years)
Adolescence marks a critical period of physical, emotional, and social development. The 99384 code is used for well-child exams during this transformative stage, which often includes:
-
Addressing puberty-related concerns and tracking secondary sexual characteristics (Tanner Staging).
-
Discussion of mental health and emotional well-being, including screening for depression, anxiety, or risky behaviors.
-
Education on topics such as substance use, sexual health, and peer pressure.
-
Immunizations specific to this age group, such as HPV, meningococcal, and Tdap vaccines.
-
Physical examination to monitor growth, weight, BMI, and potential sports-related concerns.
CPT Code 99385: Well Child Exam for Young adults (ages 18–39 years)
This code applies to young adults transitioning into independent healthcare. Although the focus shifts somewhat from pediatric concerns, preventive care remains a priority. This visit typically involves:
-
A detailed review of lifestyle habits, including diet, exercise, and substance use.
-
Counseling on sexual health, family planning, and prevention of sexually transmitted infections (STIs).
-
Screening for chronic conditions like hypertension, obesity, or diabetes, especially in individuals with risk factors.
-
Immunization updates, such as annual flu shots or catch-up vaccines if any were missed during adolescence.
-
Health education to promote long-term wellness and proactive care, including stress management and work-life balance.
Well Child CPT Codes for Established Patients
For established patients, who have previously visited the practice, CPT codes 99391–99395 are used to document well-child exams
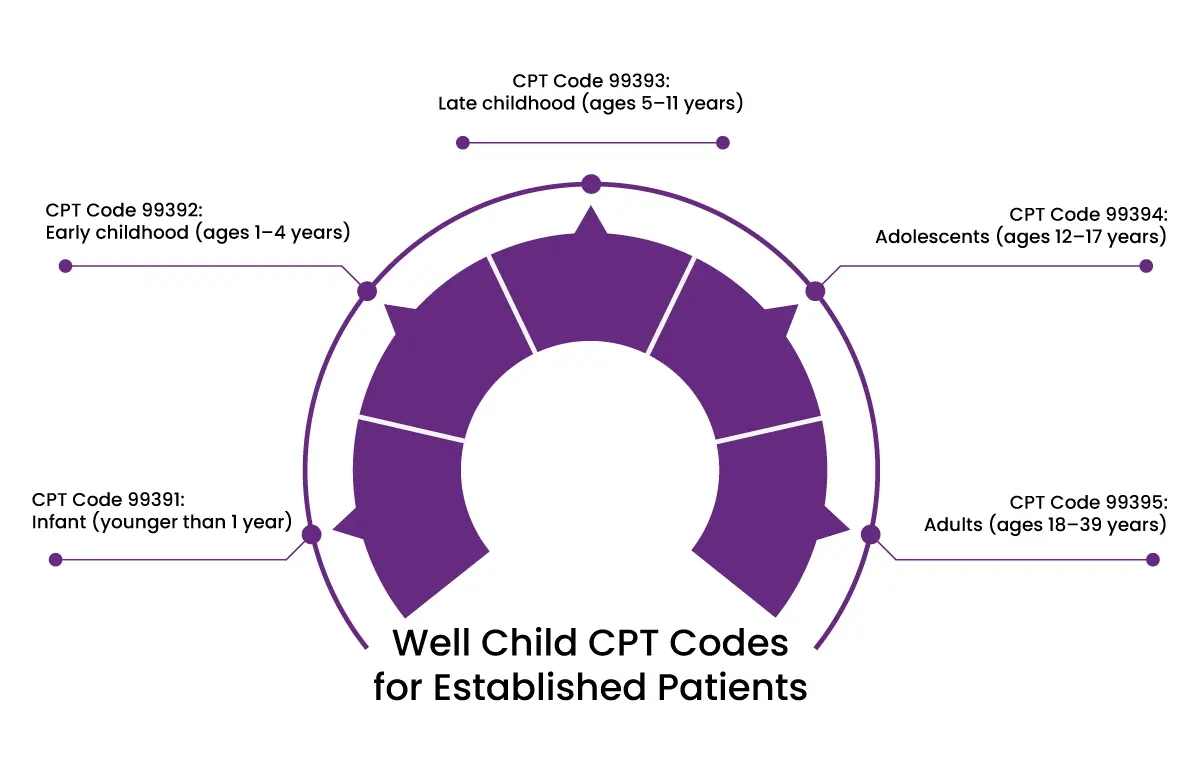
CPT Code 99391: Infant (younger than 1 year)
Covers follow-up visits for infants, including tracking growth metrics such as weight, length, and head circumference. The visit ensures adherence to the immunization schedule and addresses any emerging concerns regarding feeding or development.
CPT Code 99392: Early childhood (ages 1–4 years)
Focuses on age-appropriate screenings, including developmental milestones such as motor skills and speech. Immunization updates and guidance for parents on safety measures, nutrition, and behavioral concerns are key components of this visit.
CPT Code 99393: Late childhood (ages 5–11 years)
Emphasizes growth tracking (height, weight, BMI) and academic readiness, including discussions about school performance. Routine checks for conditions such as scoliosis or vision issues and booster vaccines are included.
CPT Code 99394: Adolescents (ages 12–17 years)
Addresses physical and emotional changes during puberty. Includes discussions about mental health, risky behaviors, and lifestyle habits. Vaccinations, such as HPV and meningococcal boosters, are updated as needed.
CPT Code 99395: Young adults (ages 18–39 years)
Covers preventive care for young adults transitioning to independent healthcare. Focus areas include screenings for chronic conditions, lifestyle counseling, and sexual health education. Immunization status is reviewed and updated.
What If Abnormality Is Discovered During a Well-Child Exam?
When an abnormality or illness is discovered during a well-child exam, healthcare providers must follow specific documentation and coding guidelines to ensure both the preventive and problem-focused components of the visit are properly captured.
Documenting the Abnormality or Illness
If a well-child exam reveals an abnormality or illness, it is essential to:
-
Clearly differentiate the preventive service from the evaluation and management (E/M) of the abnormality or illness.
-
Document the additional work done to address the issue, including history, physical examination, diagnostic tests, and counseling.
Using a Modifier
In such cases, you will need to use modifier 25 with the E/M code. This modifier indicates that a significant, separately identifiable service was provided on the same day as the preventive service.
For example:
-
Report the preventive CPT code (e.g., 99383) for the well-child exam.
-
Use an appropriate E/M code (e.g., 99213) to document the additional evaluation and management work for the illness or abnormality.
-
Append modifier 25 to the E/M code to indicate that it is a separate service
Pairing with the Right Diagnosis Codes
-
Use Z-codes for the preventive service, such as Z00.121 (well-child visit with abnormal findings).
-
Add a specific ICD-10 diagnosis code for the condition discovered during the visit (e.g., J06.9 for an upper respiratory infection or H65.3 for otitis media).
Practical Example
A 6-year-old child comes in for a routine well-child exam, coded as 99393. During the visit, the provider diagnoses an ear infection. The following would be billed:
-
99393 – Well-child exam (preventive care) with Z00.121.
-
99213-25 – E/M for the ear infection, with the diagnosis code H65.3 for otitis media.
Final Words
Lastly, it goes without saying that by understanding the differences between new and established patient codes, knowing when to use modifiers, and pairing CPT codes with the correct ICD-10 diagnosis codes, healthcare providers can streamline their billing processes and minimize claim denials. A clear, compliant approach to documentation supports both the health of your young patients and the financial stability of your practice. For a distinct approach to pediatric billing, providers can partner with HMS USA LLC. Let the experts handle your billing needs, so you can focus on delivering exceptional care to your young patients.
ABOUT AUTHOR

Pedro Collins
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.