Have you ever felt like your medical practice isn't getting fairly compensated for the extra time and effort that goes into complex cases? You meticulously document every step, every decision, every unexpected turn. But when the reimbursement check arrives, it feels... underwhelming.
There's a little-known secret in medical billing that could significantly boost your practice's revenue. It's a simple code, just two digits, but it packs a powerful punch.
We're talking about Modifier 22. If you're not using it strategically, you're leaving money on the table. This guide will reveal everything you need to know about Modifier 22, from when to use it to how to document your cases for maximum reimbursement.
What is Modifier 22?
Modifier 22 is a two-digit code used in medical billing to indicate that a procedure or service requires increased procedural services. This means that the work involved was substantially greater than what is typically expected for that specific procedure.
Here's what that means in simpler terms:
-
More Time: The procedure took much longer than usual.
-
More Difficulty: The procedure was more complex or challenging than normal.
-
More Resources: The procedure required extra tools, supplies, or staff assistance.
-
Patient Condition: The patient's health condition made the procedure more difficult.
Appropriate Usage of Modifier 22
Modifier 22 is not a free pass to higher reimbursement. It should only be used in specific situations where the work performed goes above and beyond what's typically expected for a given procedure.
Here's when Modifier 22 is appropriate:
Complex Surgeries: Procedures with unexpected complications, difficult anatomy, or multiple surgeries at once.
Extensive Trauma: Treating severe injuries that require more time and resources.
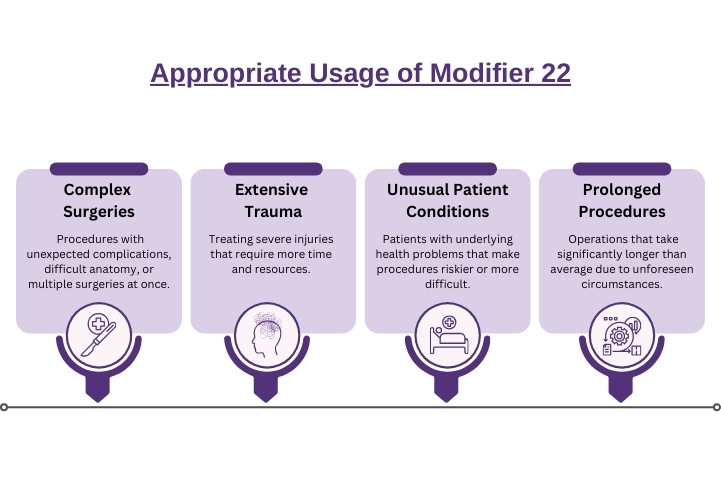
Unusual Patient Conditions: Patients with underlying health problems that make procedures riskier or more difficult.
Prolonged Procedures: Operations that take significantly longer than average due to unforeseen circumstances.
Example Scenarios for Modifier 22
A patient presents with symptoms of acute appendicitis. The surgeon schedules an appendectomy, a procedure that typically takes about an hour to complete. However, during the surgery, the surgeon discovers extensive adhesions (scar tissue) from previous abdominal surgeries. These adhesions obscure the appendix and make it difficult to access.
The surgeon must now carefully dissect through the adhesions to reach the appendix, a process that requires meticulous attention to detail and carries a higher risk of complications. This unexpected difficulty significantly extends the duration of the surgery to three hours.
In this scenario, Modifier 22 is appropriate because the presence of extensive adhesions significantly increased the complexity of the procedure. The surgeon had to perform additional work that was not anticipated based on the initial diagnosis, and the prolonged duration of the surgery justifies the use of Modifier 22.
Modifier 22 Documentation Requirements
Thorough documentation is crucial to successfully using Modifier 22 and ensuring appropriate reimbursement. According to Modifier 22 guidelines, your documentation should paint a clear picture of why the procedure or service required significantly more work than usual. This means detailing the specific factors that led to the increased procedural services.
Here's what your documentation should indicate:
-
Detailed operative notes: Include a step-by-step description of the procedure, highlighting any unexpected complications, anatomical challenges, or additional techniques used.
-
Time: Document the actual time spent on the procedure, compared to the typical duration for that specific code.
-
Resources: Note any additional tools, equipment, supplies, or staff assistance required due to the complexity of the case.
-
Patient's condition: Explain how the patient's underlying health issues or unique anatomy contributed to the increased procedural services.
-
Supporting documents: Include relevant lab results, imaging reports, pathology reports, or any other documents that can corroborate your claims.
Important Considerations:
-
Payer Requirements: Be aware that payers often request additional documentation to support the use of Modifier 22. Be prepared to provide any requested information promptly.
-
Provider Statement: Some payers may require a separate statement from the provider explaining why the service was prolonged or complex. This statement should clearly articulate the factors that differentiated this case from a standard procedure.
-
Convincing Evidence: Your documentation must be detailed, specific, and convincing. Vague or generalized statements will not be sufficient to justify the use of Modifier 22.
Timeliness:
It's crucial to document the details of the procedure as soon as possible while the information is still fresh in your mind. Delaying documentation can lead to errors or omissions, which could weaken your case for increased reimbursement.
Inappropriate Use of Modifier 22
It's crucial to understand when not to use Modifier 22. Incorrect use can lead to claim denials and delays in reimbursement.
Avoid using Modifier 22 for:
-
Evaluation and management (E/M) services: These are separate services with their own billing codes.
-
Anesthesia services: Anesthesia is billed separately with specific codes and modifiers.
-
Durable medical equipment (DME): DME is billed with HCPCS codes and does not typically warrant Modifier 22.
-
Unlisted codes: Unlisted codes already lack a specific definition, so adding Modifier 22 would be redundant.
Additionally, Modifier 22 is NOT appropriate in the following situations:
-
Surgeon's choice: If the procedure is prolonged or complicated solely because of the surgeon's preferred approach, not due to unexpected circumstances or the patient's condition.
-
Expected adhesions: When the extent of adhesions requiring lysis is typical for that procedure, it should be included in the primary procedure code.
-
Robotic assistance: Simply using a robotic-assisted technique does not automatically justify Modifier 22 unless the procedure itself was significantly more complex or time-consuming.
If Modifier 22 is used inappropriately, payers may deny the claim outright. If a more specific code exists to describe the services performed, they may deny the use of Modifier 22 and request that you rebill using the more appropriate code.
Remember, thorough documentation is crucial to justify the use of Modifier 22. If you are unsure whether it's appropriate in a particular situation, it's always best to consult with a coding expert or seek clarification from the payer.
Final Words
Modifier 22 is an important role for medical providers aiming to receive proper compensation for complex procedures and increased procedural services. . By understanding when and how to use Modifier 22 correctly, along with meticulous documentation, you can optimize your billing and ensure you're accurately compensated for the full scope of your work.
Partnering with a medical coding and billing specialist can be an effective way to ensure accuracy and efficiency in your billing processes. HMS USA LLC offers expertise in medical coding and modifiers, including Modifier 22. If you're looking to streamline your billing and maximize your reimbursement, consider exploring the services available from a specialized provider like HMS USA LLC.
ABOUT AUTHOR

John Wick
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.