The old adage, "Two heads are better than one," rings especially true in healthcare. The healthcare landscape is rapidly shifting away from the traditional fee-for-service model, where the quantity of care trumped quality. Today, the spotlight is on value-based care—a model that rewards providers for delivering better patient outcomes, not just more services.
This makes CINs (Clinically integrated networks) to be at the forefront of a monumental shift toward value-based care. Are you ready to move beyond the limitations of the fee-for-service model and embrace a future of collaborative, data-driven care? Let's dive deeper into how CINs work, the benefits they offer, and the steps you can take to join one.
What is a Clinically Integrated Network (CIN)?
A Clinically Integrated Network (CIN) is a formal collaboration among a diverse group of healthcare providers, including hospitals, physicians (both employed and independent), specialists, and other healthcare organizations. The unifying goal of a CIN is to enhance patient care by improving coordination, quality, and efficiency while reducing unnecessary costs.
7 Components of a CIN:
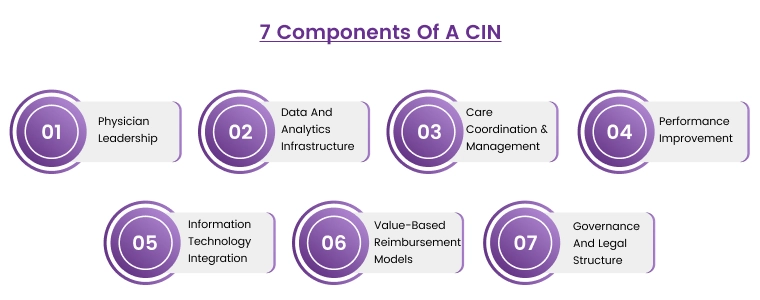
Physician Leadership: Strong physician leadership is the cornerstone of successful clinical integration. Physician leaders must actively participate in the development and implementation of clinical protocols, quality improvement initiatives, and governance structures. Their engagement fosters trust and collaboration among providers.
Data and Analytics Infrastructure: A robust data infrastructure is essential for collecting, analyzing, and sharing patient data. CINs rely on data to track performance, identify trends, and measure the effectiveness of interventions. Advanced analytics tools can help identify high-risk patients, predict outcomes, and guide care management decisions.
Care Coordination and Management: CINs emphasize care coordination to ensure patients receive timely, appropriate care across the continuum. This involves developing standardized care pathways, implementing care management programs for chronic conditions, and facilitating communication among providers.
Performance Improvement: Clinical integration focuses on continuous quality improvement. This includes setting performance goals, measuring provider performance against benchmarks, identifying areas for improvement, and implementing evidence-based interventions to enhance care quality and outcomes.
Information Technology (IT) Integration: Integrated IT systems facilitate seamless data sharing, communication, and care coordination among providers. Electronic health records (EHRs), clinical decision support tools, and patient portals are essential components of a well-functioning CIN IT infrastructure.
Value-Based Reimbursement Models: CINs often participate in value-based payment models, such as ACOs or bundled payment programs. These models reward providers for achieving quality targets and improving patient outcomes, incentivizing collaboration and cost-effective care delivery.
Governance and Legal Structure: CINs require a well-defined governance structure to ensure effective decision-making, resource allocation, and conflict resolution. The legal structure of the CIN must comply with antitrust laws and regulations to avoid anti-competitive behavior.
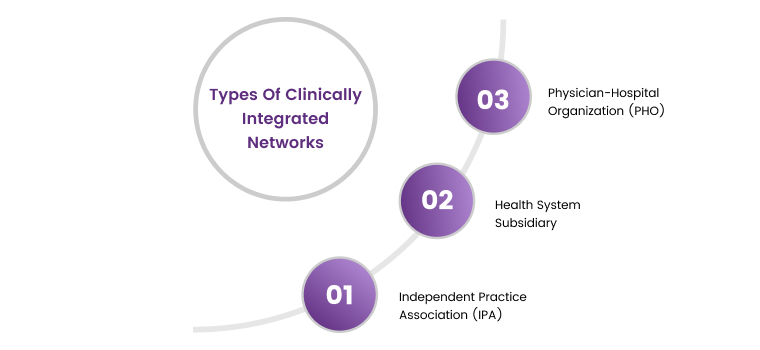
Types of Clinically Integrated Networks?
Clinically Integrated Networks (CINs) can take on various forms, each with its own structure and characteristics. Here are the main types:
-
Physician-Hospital Organization (PHO): This is a common type of CIN where physicians and hospitals partner to create a joint venture. PHOs can be owned jointly by both parties or solely by the hospital, but they always involve shared governance and decision-making.
-
Health System Subsidiary: In this model, the CIN is a subsidiary or division of a larger health system or integrated delivery network (IDN). This allows for close integration with existing infrastructure, resources, and care coordination mechanisms.
-
Independent Practice Association (IPA): An IPA-based CIN is comprised solely of independent physician practices. This allows physicians to maintain their independence while benefiting from the collective bargaining power, shared resources, and care coordination efforts of the CIN.
Are CINs and ACO Same?
Clinically Integrated Networks (CINs) and Accountable Care Organizations (ACOs) are closely related concepts in healthcare, but they are not interchangeable. Both share a common goal: improving patient care while lowering costs through collaboration among diverse healthcare providers.
However, there are some key distinctions:
-
Focus: CINs primarily focus on clinical integration, meaning the alignment of clinical processes, care coordination, and quality improvement across the network. ACOs, on the other hand, emphasize financial accountability for a defined population of patients. This means they are responsible for both the quality and cost of care for their assigned patients.
-
Structure: A CIN is a distinct legal entity, often structured as a physician-hospital organization (PHO), an independent practice association (IPA), or a subsidiary of a health system. An ACO is also a legal entity, but it contracts with payers (e.g., Medicare, commercial insurers) to provide coordinated care to a specific patient population.
-
Purpose: While both CINs and ACOs aim to improve patient outcomes and reduce costs, CINs often serve as a foundation for ACOs. By establishing the necessary infrastructure for care coordination and quality improvement, CINs can facilitate the formation and success of ACOs in value-based payment models.
In essence, you can think of CINs as the collaborative network of providers working together to enhance care delivery, while ACOs are the formal structure that takes on financial risk and accountability for a defined patient population. ACOs often rely on the clinical integration achieved within a CIN to meet their goals.
It's worth highlighting that while all ACOs can be considered clinically integrated, not all CINs operate as ACOs. Some CINs may choose not to participate in value-based payment models and focus solely on improving clinical integration within their network.
The CIN Advantage To Healthcare Providers
At the core of clinically integrated networks (CINs) is a shared commitment to achieving the Institute for Healthcare Improvement's (IHI) "Triple Aim. By working towards the Triple Aim, CINs position themselves as healthcare leaders. Here's how:
Expertise and Superior Care
CINs demonstrate to payers (insurance companies) that they have the expertise and infrastructure to deliver better care at a lower cost. This is achieved through the coordinated efforts of their network, including data-driven decision-making, shared best practices, and streamlined care processes.
Negotiating Power
This proven ability to provide superior care gives CINs greater leverage when negotiating reimbursement rates with payers. They can secure more favorable contracts and higher payment rates for their members.
Transparent Coordination
The collaborative nature of CINs fosters transparency and data sharing among health systems and providers. This leads to smoother care transitions, fewer duplications of services, and improved communication, ultimately benefiting patients.
Mutual Accountability
CINs create a system of mutual accountability where all members are invested in achieving the Triple Aim. This encourages everyone to work together efficiently and effectively to deliver the highest quality care.
Independence with Collaboration
CINs offer a unique advantage for independent practices. They allow practices to remain independent while tapping into a wider network of resources, expertise, and collaborative opportunities.
Final Words
Clinically integrated networks (CINs) are not just about improving healthcare; they are about transforming it. By focusing on the Triple Aim, they create a system that benefits patients, providers, and payers alike. The collaboration, data-driven decision-making, and commitment to quality that characterize CINs are key to handling the complexities of the modern healthcare landscape and achieving sustainable success.
ABOUT AUTHOR

John Wick
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.
