Healthcare providers no matter dealing with any type of specialty came across some challenges and problems in terms of medical billing. One of the most common problem they face is an error or a denial sent by the insurance payers about entity that is billing for services.
Grasping the concept of an entity code in medical billing and recognizing how its accurate use can streamline claims and billing procedures is of paramount importance. Some time it is very common that you receive a denial from an insurance payer saying that “this code requires the use of an entity code” and you are left scratching your head out what is an entity code?
So to get out of most of your answers about entity code in medical billing, you can't miss our must read blog. Before diving deep inside into the further detail of the coding errors, let’s start with discussing what exactly is mean by entity in medical billing?
What is an Entity in Medical Billing?
The term "entity" refers to a person, place, or thing that possesses an independent existence. Similar to how a company and the individuals within it are considered entities, the concept holds true in the context of medical billing.
When we discuss entities in medical billing, it encompasses a broad spectrum. Patients who receive medical services are recognized as entities, and the services provided to these patients by healthcare providers also fall under this category. Interestingly, even if you've outsourced your medical billing functions to a third-party team, they too are designated as entities within this framework.
The term "entity" holds substantial importance in the realm of medical billing due to its implication of relationships within the landscape of healthcare services. It extends its reach to encompass any controlled liability company that is directly or indirectly engaged in the process of medical billing services.
This crucial piece of information plays a pivotal role in the precise generation of codes for patient visits and the seamless collection of payments from insurance companies on behalf of healthcare providers.
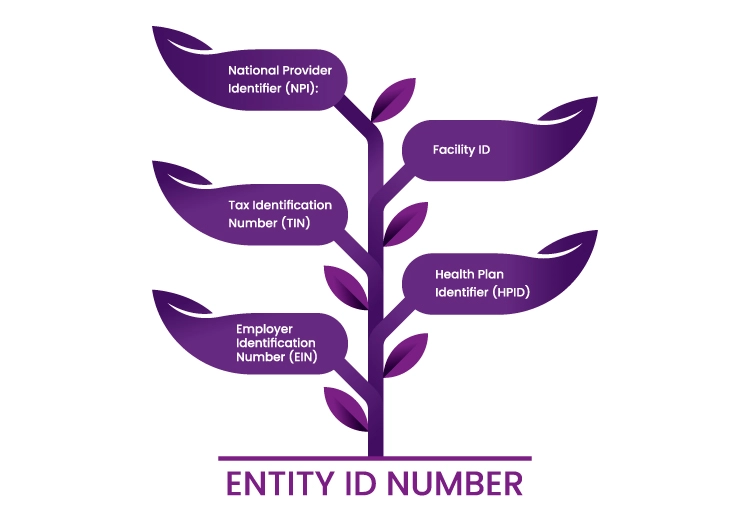
What is an entity Id number?
An "Entity ID Number" generally refers to a unique identifier assigned to a specific entity within a particular system or organization. In the context of medical billing or healthcare administration, an Entity ID Number could refer to a unique identifier assigned to various entities involved in the healthcare process. These entities could include healthcare providers, medical facilities, insurance companies, and more.
The term "Entity ID Number" itself does not specify a specific format or length for the identifier; it could be a numeric, alphanumeric, or even a combination of letters and numbers, depending on the system's requirements.
For example:
National Provider Identifier (NPI): This is a type of Entity ID Number used in the United States for healthcare providers. It's a 10-digit numeric identifier assigned to individual providers and organizations involved in healthcare.
Tax Identification Number (TIN): This is another type of Entity ID Number used for tax purposes, and it's assigned to businesses, including healthcare facilities.
Employer Identification Number (EIN): Similar to TIN, EIN is used to identify businesses, including healthcare organizations, for tax purposes.
Facility ID: Healthcare facilities might have their own internal identifier or Facility ID for administrative and billing purposes.
Health Plan Identifier (HPID): This is an identifier used to uniquely identify health plans, including insurance companies, in electronic healthcare transactions.
What are common entity related errors in billing claim?
The most common reason of entity code errors is that health care providers may submit the wrong npi or tax identification number (equivalent to box 33 on the CMS claim form 1500). Some of the other errors that are related to entities are:
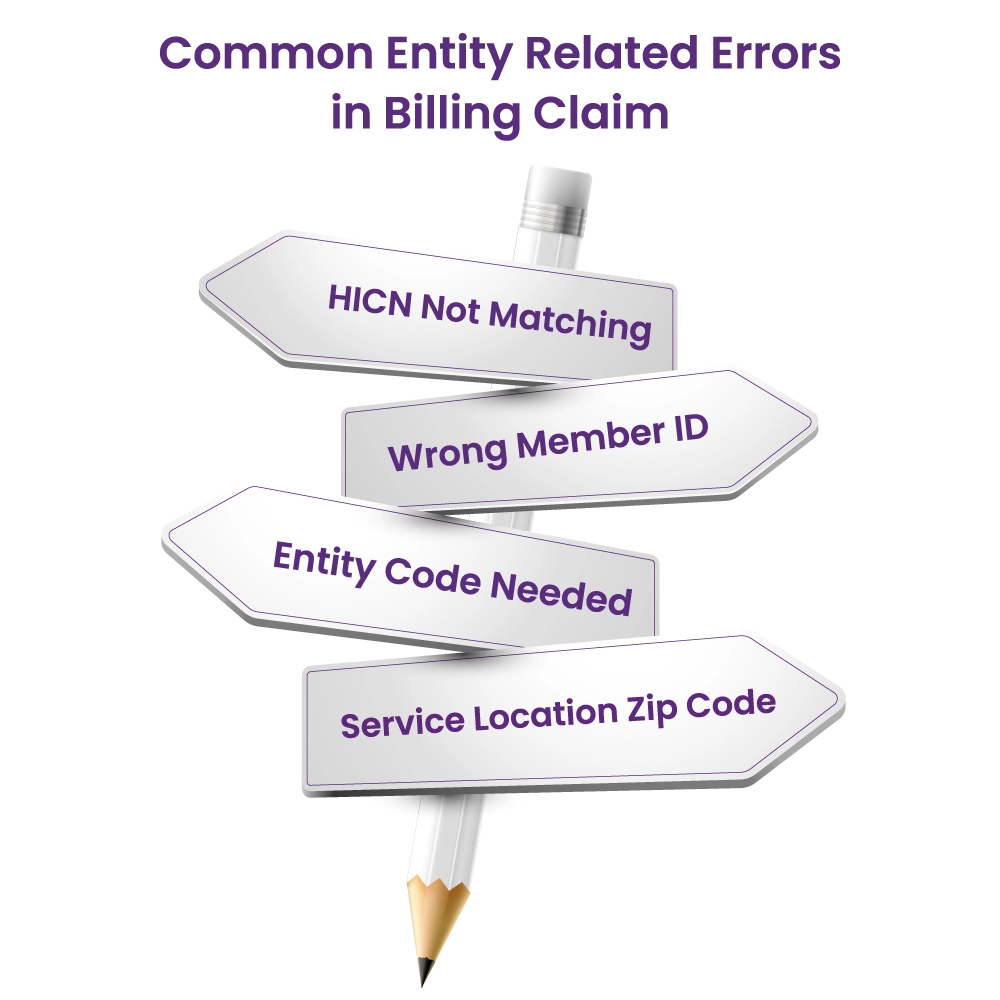
HICN Not Matching
This happens when there's a mistake with the Health Insurance Claim Number (HICN). This mistake often comes up when a claim is corrected and sent again. The entity here is the insurance payer. To fix this, the biller needs to make sure they use the same claim number given by the payer for the first submission.
Wrong Member ID
This mistake happens when there's missing information about the patient. It can also happen if the patient's insurance changed or if they weren't covered when they got the service. Sometimes, this mistake shows up if the claim went to the wrong insurance company because the patient's ID doesn't match.
Entity Code Needed
This happens when the biller didn't clearly identify an entity in the claim. So, the biller needs to check all the parts of the claim – patient, provider, and any other doctors involved – to make sure everything's clear.
Service Location Zip Code
This error is about the provider's location. The biller needs to put the last four numbers of the zip code, not just "0000." If this mistake comes up, it means the zip code is incomplete.
What is the entity code denial?
An entity code denial happens when the insurance payer receives a claim but encounters a problem with the entity codes involved. This could be due to discrepancies or inaccuracies in how the entity codes are applied. The denial notice typically provides information about the denial reason, which could range from incorrect entity code assignment to missing or mismatched entity information.
Implications and Resolutions
Entity code denials can have significant implications for both healthcare providers and patients. They can lead to delays in claims processing, payment disruptions, and increased administrative work. To resolve an entity code denial, the biller or provider needs to identify the specific issue with the entity codes and rectify it. This might involve cross-referencing codes, verifying entity information, and ensuring accurate data entry.
Preventing Entity Code Errors
Prevention is often the best approach when it comes to entity code errors. Healthcare providers can significantly reduce the occurrence of these errors by adhering to best practices. Here are essential steps to consider:
1. Accurate Payer ID Submission
Before submitting a claim, ensure the accuracy of the payer ID number. This crucial step involves verifying the payer ID and making corrections if any errors are identified. Double-checking this identifier helps prevent confusion and reduces the likelihood of entity code errors.
2. Precise Patient Demographic Information
Accurate patient demographic details play a pivotal role in claims processing. Ensure that you enter correct information, including the patient's residence, member ID, and other relevant details. Taking the time to verify this information can mitigate errors arising from mismatched or incomplete patient data.
3. Verification of Patient's Insurance Policy
In cases where a patient has been newly added to an insurance policy or experienced changes in coverage, thorough verification becomes crucial. Take proactive steps to confirm the patient's insurance status and coverage details. This action ensures that claims are submitted under the correct insurance policy, reducing the risk of denials due to coverage discrepancies.
4. Attention to Admission Criteria
For inpatient services, it's essential to adhere to admission criteria. Verifying and documenting patient admission details accurately ensures that claims reflect the appropriate level of care provided. This step contributes to correct coding and billing, minimizing errors stemming from discrepancies in service descriptions.
Final Words
In conclusion, grasping the importance of entity codes in medical billing is vital for seamless claims processing. Errors in entity codes can lead to denials and administrative complications. Adhering to best practices is key to preventing these issues. For expert assistance in navigating entity code complexities, healthcare providers can turn to HMS USA LLC. Their specialized knowledge can enhance billing accuracy and streamline financial workflows, benefiting both providers and patients.
ABOUT AUTHOR

Shahab ud Deen
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.