Have you ever found yourself tangled in the web of billing complexities instead of focusing on what you do best—caring for patients? In the bustling field of healthcare, where every moment counts, dealing with the complexities of billing can often feel like an unnecessary headache.
What if I told you there’s a way to shed this burden and refocus on your patients? You can achieve this by outsourcing your medical billing tasks to a third-party billing provider. So, before diving into the world of third-party medical, let's see what third-party billing is.
What is Third Party Medical Billing?
Third-party billing refers to the process of outsourcing the management of a healthcare provider's billing and claims processes to an external company specialized in handling these functions.
This includes a wide range of services, from generating invoices for services rendered to submitting claims to insurance companies and following up on payments. The goal of third-party billing is to ensure that healthcare providers are reimbursed accurately and in a timely manner for the care they provide to their patients.
Challenges Faced Due to In-House Billing
Transitioning from the broad overview of third-party billing, it becomes crucial to understand why many healthcare providers are moving away from in-house billing operations. Despite the best intentions, managing billing and claims processing internally can introduce several challenges that may impact both the efficiency of healthcare services and the financial stability of the practice.
1. Complexity of Medical Billing and Coding:
The medical billing and coding landscape is notorious for its complexity, with thousands of codes for diagnoses, treatments, and procedures that must be accurately applied. In-house staff must stay abreast of the latest updates and changes to these codes, a task that is both time-consuming and prone to errors. Mistakes in coding can lead to claim denials or delays, affecting cash flow and revenue.
2. Staffing Issues:
Maintaining an in-house billing department requires hiring specialized staff who are skilled in medical billing and coding. This poses challenges in terms of recruitment, training, and retention. Furthermore, staff absences due to sickness or vacation can disrupt the billing process, leading to delays in claim submissions and reimbursements.
3. Increasing Administrative Burden:
Healthcare providers face a growing administrative burden, with more time spent on paperwork and less on patient care. The administrative tasks associated with in-house billing, such as claim submission, follow-up, and dealing with insurance companies, can be overwhelming and detract from the core mission of providing quality healthcare.
4. Compliance and Regulatory Issues:
The healthcare industry is heavily regulated, with strict compliance requirements for billing and patient data handling. Staying compliant requires constant vigilance and understanding of the regulations, which can be a significant challenge for in-house billing staff. Non-compliance can result in penalties, legal issues, and damage to the provider’s reputation.
5. Financial Inefficiencies:
In-house billing often leads to higher operational costs, including salaries, benefits, training, and billing software. Additionally, inefficiencies and errors in the billing process can result in delayed payments, claim rejections, and the need for resubmissions, further straining the financial health of the practice.
6. Focus Shift from Patient Care:
Perhaps the most significant impact of managing billing in-house is the shift in focus from patient care to administrative tasks. Healthcare providers may find themselves caught up in managing the billing process, which can compromise the quality of care and patient satisfaction.
What Billing Process Does A Third Party Billing Provider Follow?
For streamlined billing operations, most third-party billing providers adhere to a comprehensive Revenue Cycle Management (RCM) cycle. This approach is designed to ensure that healthcare billing and claims are managed with precision and efficiency. The process breakdown is as follows:
1. Patient Check-in and Verification: The process begins at patient check-in, where the third-party billing provider ensures that all patient information is accurately recorded and verified. This includes personal details, insurance information, and the purpose of the visit. Accurate information at this stage is crucial for smooth billing and claims processing.
2. Coding of Services: After the healthcare service is provided, the third-party billing service codes the services rendered. This involves translating the diagnoses and procedures into standardized codes recognized by insurance companies. The accuracy of coding is paramount to avoid denials or delays in reimbursement.
3. Claim Submission: With the services coded, the next step is to submit the claim to the relevant insurance company. Third-party billing providers use specialized software to electronically submit claims, speeding up the process and reducing the likelihood of errors compared to manual submissions.
4. Monitoring and Follow-ups: Submitting the claim is not the end of the road. The third-party billing provider actively monitors the status of each claim, following up with insurance companies as needed. This proactive approach helps in addressing any issues that may arise, such as denials or requests for additional information, ensuring that claims are processed as quickly as possible.
5. Payment Posting and Reconciliation: Once a claim is approved, the insurance company disburses the payment. The third-party billing provider then posts these payments against the respective patient accounts, ensuring that all financial records are up-to-date. They also reconcile any discrepancies between the billed amounts and the payments received.
6. Patient Billing for Outstanding Balances: If patients have responsibilities, such as co-pays or deductibles, the third-party billing provider will generate and send statements to patients for the outstanding balances. They also handle any patient inquiries related to billing, providing clear and concise explanations of charges.
7. Reporting and Analytics: Third-party billing providers often offer comprehensive reporting and analytics services, giving healthcare providers insight into their billing processes, financial performance, and areas for improvement. These reports can help in making informed decisions about the practice’s operations and financial planning.
Benefits of Outsourcing Healthcare Finances to a Third-Party Medical Billing Company
Outsourcing healthcare finances to a third-party medical billing company can significantly transform the operational dynamics of a healthcare provider. This strategic move is not just about delegating tasks; it's about enhancing the healthcare practice's efficiency, accuracy, and profitability. Here are some key benefits:
Enhanced Focus on Patient Care
Key Insight: Outsourcing liberates healthcare providers from the maze of billing, enabling an undiluted focus on patient care, enhancing both satisfaction and outcomes.
Minimized Billing Errors and Maximized Compliance
Expertise: Specialization in medical billing nuances reduces errors, ensuring compliance with the latest regulations, thus decreasing claim denials.
Compliance Assurance: Rigorous adherence to healthcare billing regulations, including HIPAA, safeguards against compliance violations.
Accelerated Cash Flow and Cost Efficiency
Cash Flow Improvement: Expedited billing cycles result in quicker reimbursements, bolstering the financial pulse of healthcare practices.
Operational Cost Savings: Eliminates the overhead costs associated with an in-house billing department, including staff salaries and technology investments.
Technological and Professional Leverage
Access to Advanced Tech: Immediate access to state-of-the-art billing technologies and analytics without direct investment.
Scalable Solutions: Flexibility to scale billing operations in line with practice growth, without the logistical challenges of expanding an in-house team.
Security and Patient Satisfaction
Data Security: High-grade security measures protect sensitive patient data, mitigating the risk of breaches.
Customer Service Excellence: Dedicated handling of billing inquiries by specialists improves patient satisfaction through efficient and knowledgeable responses.
Insightful Reporting for Informed Decision-Making
Analytics and Reporting: Comprehensive financial analytics and reporting offer valuable insights, empowering healthcare providers to make strategic decisions.
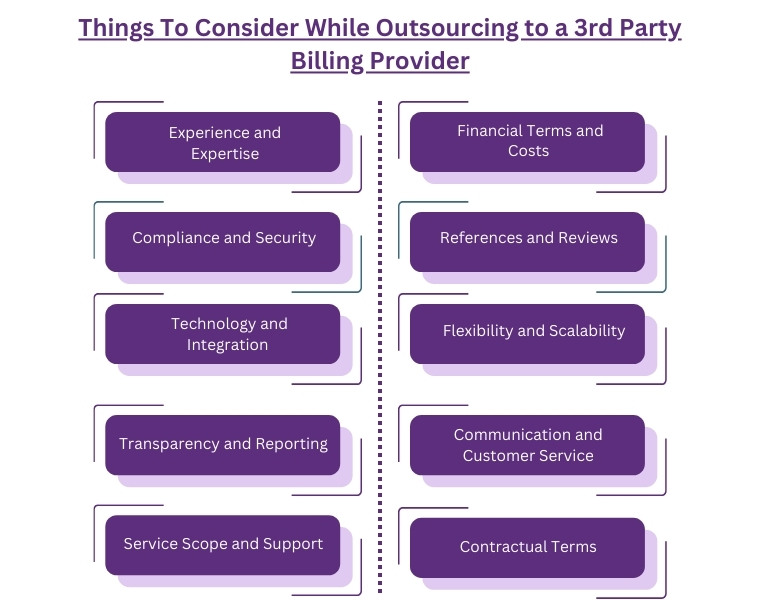
Things To Consider While Outsourcing to a 3rd Party Billing Provider
When considering outsourcing your healthcare practice's billing to a third-party provider, it's crucial to approach the decision with diligence and strategic foresight. Choosing the right partner not only affects your financial bottom line but also impacts patient satisfaction and compliance with healthcare regulations. Here are key factors to consider:
 \
\
1. Experience and Expertise: Look for a provider with a strong track record in healthcare billing within your specific field of medicine. Their experience can be a critical factor in navigating the complexities of medical billing and coding accurately.
2. Compliance and Security: Ensure the billing provider is fully compliant with all healthcare regulations, including HIPAA. They should have robust security measures in place to protect patient data and guard against data breaches.
3. Technology and Integration: Assess the technology used by the billing provider. Their systems should seamlessly integrate with your existing Electronic Health Record (EHR) system to ensure a smooth transition and continuous flow of data.
4. Transparency and Reporting: Your billing provider should offer complete transparency in their operations, providing detailed reports and analytics that give you insight into your financial performance, billing processes, and areas for improvement.
5. Service Scope and Support: Understand the full scope of services offered. Besides basic billing and coding, consider if they offer services like denial management, follow-up on unpaid claims, patient billing inquiries, and other support services. Their ability to provide comprehensive support is vital.
6. Financial Terms and Costs: Evaluate the cost structure and financial terms. Consider how the billing provider's fees are structured — whether it's a percentage of collections, a flat fee, or based on other parameters. Ensure there are no hidden fees and that the terms align with your practice's financial goals.
7. References and Reviews: Seek references and check reviews from other healthcare providers. Hearing about others' experiences can provide invaluable insights into the provider's reliability, efficiency, and customer service quality.
8. Flexibility and Scalability: Consider whether the billing provider is flexible and scalable enough to accommodate your practice's growth and any changes in service needs over time.
9. Communication and Customer Service: Effective communication is key to any successful partnership. Ensure the provider has a clear communication process and is committed to promptly addressing any issues or concerns.
10. Contractual Terms: Carefully review the contractual terms, paying close attention to the length of the contract, termination clauses, and any obligations or penalties involved in ending the partnership.
Wrapping Up
Choosing the right third-party billing provider is a significant decision that can influence your practice’s operational efficiency, financial health, and patient satisfaction levels. Thoroughly evaluating potential providers based on these considerations can help ensure a successful and beneficial partnership.
ABOUT AUTHOR

Neil Wagner
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well-researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.