In the field of medical billing, the process of billing for behavioral health services has proven to be a complex and challenging task for providers. With the increasing demand for specialized mental health care, it has become imperative for providers to have a specialized billing system in place that can effectively manage all relevant medical Current Procedural Terminology (CPT) codes and associated services.
It is a common misconception that behavioral health billing and traditional medical billing are identical. However, this is not the case, as behavioral health billing involves unique coding and reimbursement requirements that differ from conventional medical billing. Therefore, it is crucial for providers to understand the complexities of behavioral health billing and to have a billing system specifically designed to handle the unique requirements of behavioral health services.
Contents
Why Is Behavioral Health Billing Considered To Be Complex?
Coding Regulations for billing behavioral health services
Specialty Services Covered Under Behavioral Health Billing
Tips for Maximizing Reimbursement Using Professional Billing Service
Why Is Behavioral Health Billing Considered To Be Complex?
Behavioral health billing is considered to be complex for several reasons:
Firstly, there is a unique set of coding requirements for behavioral health services, which are different from traditional medical billing codes. This requires a specialized understanding of behavioral health billing codes and their proper application.
Secondly, behavioral health services often involve multiple levels of care, including outpatient therapy, inpatient hospitalization, and partial hospitalization. Each level of care has its own set of coding requirements, which can further complicate the billing process.
Thirdly, insurance coverage for behavioral health services varies widely, with some insurance plans providing limited coverage for mental health services and others providing more comprehensive coverage. This variability can make it difficult for providers to bill for behavioral health services accurately and to determine the appropriate reimbursement rate.
Fourthly, strict regulations and guidelines often govern the provision of behavioral health services. The billing process must comply with these regulations to avoid potential legal and financial penalties.
Coding Regulations for Billing Behavioral Health Services
Billing for mental and behavioral health services encompasses much more than just the diagnosis and Current Procedural Terminology (CPT) codes. These types of medical billing require a specialized understanding due to the significant differences that can lead to confusion for inexperienced billers.
The submission of claims for behavioral health services can vary from one payer to another, highlighting the importance of adhering to the regulations and codes specific to the services rendered and the guidelines of the patient's insurance plan.
Evaluation and Management (E&M) codes in behavioral health billing are more complex than those in traditional medical billing. The time associated with a visit is a critical component in the billing process for psychotherapy services and must be accurately captured and documented.
Additionally, payers may require specific codes to be submitted along with claims, and the billing professional must ensure that these requirements are met. The billing format is crucial for behavioral health services and can differ from one payer to another. This can include the CMS1500, UB-04, or electronic billing through the facility's electronic health record (EHR) system.
The strict coding regulations placed on mental and behavioral health claims ensure that the services are accurately captured and that reimbursement is received appropriately.
Most Commonly Used CPT Codes
CMS has provided a proper list of CPT codes that should be used when billing for behavioral health services, some of the most commonly used Current Procedural Terminology (CPT) codes include:
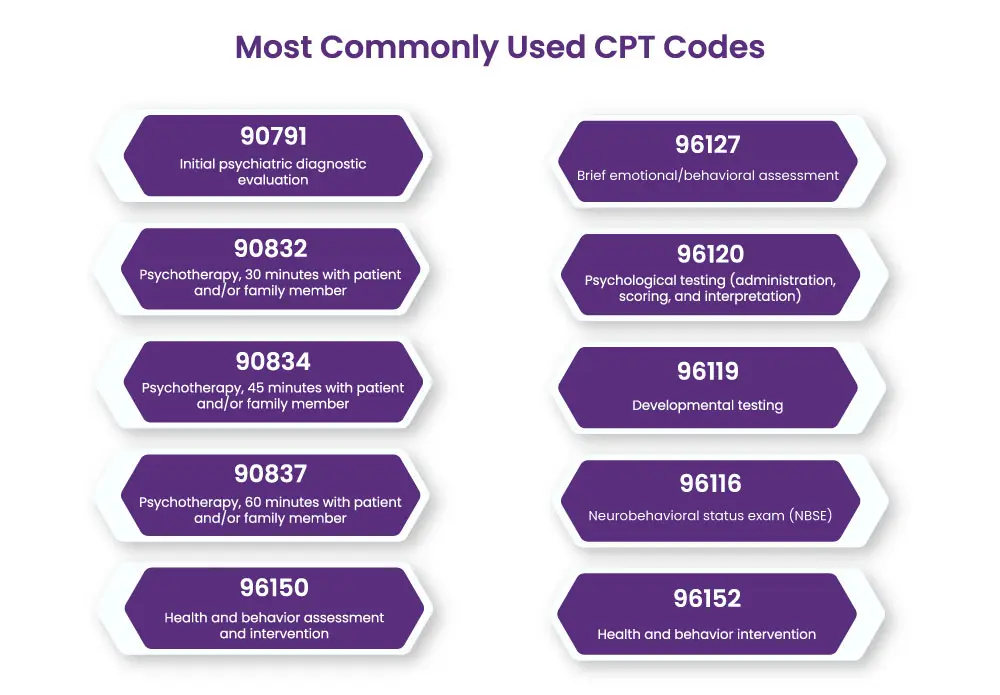
- 90791: Initial psychiatric diagnostic evaluation
- 90832: Psychotherapy, 30 minutes with patient and/or family member
- 90834: Psychotherapy, 45 minutes with patient and/or family member
- 90837: Psychotherapy, 60 minutes with patient and/or family member
- 96150: Health and behavior assessment and intervention
- 96152: Health and behavior intervention
- 96116: Neurobehavioral status exam (NBSE)
- 96119: Developmental testing
- 96120: Psychological testing (administration, scoring, and interpretation)
- 96127: Brief emotional/behavioral assessment
The specific codes used will depend on the type and length of service provided, as well as the requirements of the payer. To ensure accurate billing, providers should always verify their services' specific codes and requirements with the relevant payers.
Specialty Services Covered Under Behavioral Health Billing
Behavioral health billing has got a large domain to cover. Patients and insurance companies are mainly billed for psychiatric, psychological, and therapy services.
Psychiatry medical billing
In psychiatry billing, a few distinct coding requirements must be followed. These codes are used to accurately capture the services provided and determine the correct reimbursement rate from payers.
Psychiatry medical billing is a specialized medical billing area requiring an understanding of specialty-specific codes, guidelines, and regulations to ensure accurate claims submission.
Therapy Billing Service
Therapy billing services encompass psychiatry group therapy, individual therapy, psychological testing & assessments, family therapy, cognitive-behavioral therapy (CBT) etc.
Understanding the different coding requirements for each type of service is essential to ensure accurate billing and reimbursement. Proper documentation is necessary when submitting claims for therapy services, as the complexity of these claims can lead to confusion and decreased reimbursement if not completed correctly.
To ensure thorough and accurate billing for all types of mental and behavioral health services, it is essential to have an experienced team of professionals on hand who are knowledgeable in the regulations and codes associated with psychiatry billing, psychological and therapy billing.
Tips for Maximizing Reimbursement Using Professional Billing Service
Maximizing reimbursement for behavioral health services requires a comprehensive understanding of the specific billing requirements, regulations, and codes involved. Here are a few tips for providers looking to maximize reimbursement through professional billing services for behavioral health:
Stay up-to-date with the latest coding and reimbursement regulations: Regularly review and update your knowledge of the latest regulations and codes to ensure that you are billing correctly for the services provided.
Utilize specialized billing software: Behavioral health billing can be complex, so it's important to have the right tools in place to capture and submit claims accurately. Investing in specialized behavioral health billing software can streamline the process and improve the accuracy of claims submissions.
Partner with a professional billing service: Partnering with an experienced behavioral health billing service can help ensure that your claims are submitted accurately, promptly and in compliance with the latest regulations.
Properly document all services: Accurate and detailed documentation of all services provided is critical to maximizing reimbursement. Ensure all relevant information, including diagnosis codes, service codes, and session notes, are adequately documented and stored.
Regularly review claims submissions: Regularly review claims submissions to ensure that all services are captured and billed accurately. Address any discrepancies promptly and seek assistance from a professional billing service if necessary.
Manage patient insurance and authorization: Ensure that patients' insurance coverage is up-to-date and that all necessary authorizations have been obtained before rendering services.
By following these tips and utilizing professional billing services, behavioral health providers can improve the accuracy of their billing submissions, minimize denied claims and maximize their reimbursement for the services they provide.
Final Words
Behavioral health medical billing is a specialized and complex process that requires understanding the latest regulations, codes, documentation requirements, and reimbursement guidelines. So to get paid accurately and properly for the services you have rendered, you need to seek help from a professional provider.
So if you are not getting desired results doing searches on google regarding medical billing near me, relax and get in touch with HMS USA LLC, a top-performing company in the list of behavioral health billing companies in NY, providing specialized medical billing services to behavioral health providers.
By partnering with HMS USA LLC, you can streamline the billing process and optimize your reimbursement, freeing you to focus on what you do best – providing quality care to your patients.
ABOUT AUTHOR

Tammy Carol
As a blog writer with years of experience in the healthcare industry, I have got what it takes to write well researched content that adds value for the audience. I am a curious individual by nature, driven by passion and I translate that into my writings. I aspire to be among the leading content writers in the world.
